Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/knowledge/treatment-options/
Treatment options
We believe in a holistic, evidence-based approach to menopause treatment. Read on to learn more about a range of options to treat the symptoms of the menopause including HRT, prescribed alternatives to HRT, natural treatments, lifestyle changes, talking therapies, coaching, sex therapy, and physiotherapy.
Explore

Our clinic manages a range of issues related to the menopause. They include:
- Symptoms of the perimenopause and menopause
- Surgical or medical menopause
- Premature menopause (premature ovarian insufficiency)
- Vaginal symptoms related to the menopause
- Menopause sexual dysfunction
The starting point for our treatment is a consultation with you, where we’ll listen carefully to get a thorough understanding of the symptoms you’re experiencing and how you’re feeling. Our aim is to support you in making choices that work best for you.
We believe in a holistic and evidence-based approach to menopause treatment, which is always based on your individual symptoms and needs. It’s true that Hormone Replacement Therapy (HRT) works brilliantly for many women, but it isn’t the only solution available.
Lifestyle changes such as exercise and diet have a key role to play, and other alternative therapies can work as well. Coaching, counselling, and sex therapy can also be of great benefit, depending on your symptoms.
You can find out more about each of these below.
We know many women find that tiny changes turn into bigger benefits and can make a massive difference to their physical and mental health and wellbeing. As they say, great oaks from little acorns grow.
Hormone Replacement Therapy (HRT)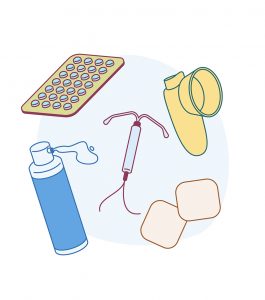
HRT is one effective way of managing symptoms that can also give long-term benefits to your bone and heart health. It’s a suitable treatment for the vast majority of women. There are small risks for some, and you’ve probably read stories in the media about links to breast cancer. However, the actual risk levels are low.
A good doctor will discuss the risks and how they might apply to you (as we do during our consultation process).
HRT can be started as early as you want in the menopause transition (perimenopause). There’s no need to wait until your symptoms become unmanageable – a single night sweat can interrupt your sleep and leave you tired and anxious the next day.
Taking HRT has a lot of benefits – it controls many symptoms of the menopause, prevents osteoporosis, and can reduce the risk of heart disease. If you experience premature menopause under the age of 40, it’s really important to take HRT until you reach the average age of the menopause (age 51 in the UK) to prevent osteoporosis and heart disease.
Over the age of 50, there’s a small increase in the risk of breast cancer for some women taking HRT, and this increases with time.
You won’t know if your menopause symptoms have settled until you stop taking HRT. Unfortunately, there is no helpful test you can do, so it’s trial and error. If you stop HRT and feel awful, don’t panic. You can usually restart it after talking to your doctor, or you can explore other options.
It’s important to remember that HRT doesn’t stop your menopause from happening. It just helps lessen the symptoms and make the transition more manageable.
Prescribed alternatives to HRT
If HRT isn’t right for you, there are other alternatives that your doctor can prescribe. Most of these aren’t intended for treating menopause symptoms, but there is evidence to support their use for specific symptoms[1].
Veoza
Veoza is a new medication licensed for the management of hot flushes and sweats. Veoza is the brand name for fezolinetant and works on the pathways in the brain responsible for the generation of hot flushes and sweats and studies have shown it’s around 60% effective at reducing the severity and frequency of vasomotor symptoms. Veoza is now available privately in the UK. Unfortunately, Veoza is not yet available on the NHS. To be available on the NHS, a further appraisal of the clinical and cost-effectiveness by the National Institute of Clinical and Healthcare Agency (NICE) is required. The publication date of this is yet to be confirmed. It is not recommended for women currently undergoing treatment for hormone dependent cancers and if you have a history of liver disease, you’ll need some tests beforehand. On the whole, it appears to be well tolerated. You can read more about Veoza here.
If you would like to discuss whether Veoza might be right for you, please book an appointment with one of the doctors in our clinic.
Clonidine
Clonidine is a blood pressure medicine that is also licensed to help with hot flushes. For some, it works wonders, but for others, it can cause dry mouth, drowsiness and can make low blood pressure even lower.
Gabapentin and Pregabalin
These medicines have a variety of uses for treating migraines, pain, anxiety, and epilepsy. Some women find they help with hot flushes and sleep (off-licence use).
Antidepressants
Antidepressants have a role to play in managing the menopause symptoms, particularly for women who have been advised not to take HRT, or do not wish to take HRT. They can be helpful in managing mood and they can help manage hot flushes and night sweats (off-licence use.)
Women taking Tamoxifen for breast cancer should be aware that some (but not all) antidepressants can make the drug less effective.
For women who can take HRT, where mood changes are related to the menopause, there is evidence suggesting that HRT is more effective in boosting mood and helping anxiety compared with antidepressants[2].
Natural treatments
Herbal remedies
Many women turn to herbal remedies before seeing a doctor for advice. If you are investigating herbal solutions, always look for the THR mark on the box. 
The Traditional Herbal Registration certification means the product has been registered by the Medicines and Healthcare products Regulatory Agency under the UK Traditional Herbal Registration Scheme.
When thinking about herbal remedies, you should consider the fact that the strength and safety are not fully known, that multiple preparation types exist and we don’t know which is the safest or best. And it’s important to know that herbal medicines can interfere with medicines that are prescribed by doctors.
Here’s a quick overview of the key herbal remedies:
- Agnus castus – commonly used for PMS. Be aware that it can negatively interact with oral contraceptives and HRT
- Black cohosh – studies have shown it can help with hot flushes. It may interact with blood pressure medicines, and you should not take it if you’re sensitive to aspirin or salicylates. It should never be taken by women taking Tamoxifen
- Evening primrose/starflower oil – these contain gamma-Linoleic acid (GLA), an essential fatty acid that helps reduce breast pain and tenderness. Be aware that GLA can increase the chance of seizure for those with epilepsy and can increase the risk of bleeding
- Ginkgo biloba – studies have shown it may have beneficial effects on memory and mental performance. Do not take it with anticoagulant drugs like warfarin and aspirin
- Sage – may help relieve hot flushes. This should not be taken by those with high blood pressure
- Sea buckthorn oil – contains omega 7 fatty acids and may help with vaginal dryness
- St John’s Wort – may be beneficial in treating anxiety and depression. St John’s Wort can make certain medicines less effective. It should not be taken with antidepressants, digoxin, warfarin, anti-asthma drugs, oral contraceptives, migraine drugs, cancer drugs, and HIV drugs. This list isn’t exhaustive – please check with a doctor if you are thinking about taking St John’s Wort
Isoflavones and phytoestrogens
Isoflavones and phytoestrogens are substances found in certain plants, like soy. They can produce a weak, oestrogen-like effect on the body. There’s evidence to suggest that women in countries where diets are traditionally rich in phytoestrogens experience fewer menopausal symptoms and have a lower rate of heart disease and osteoporosis[3].
Phytoestrogens can be taken as a supplement, such as red clover, or by increasing your intake of foods that are rich in them. Depending on your diet, you may need to radically change the way you eat to notice any effect. Phytoestrogens are not recommended for women who have had breast cancer or other hormone-dependent tumours.
Soya, linseed oils, and red clover are the richest food sources of phytoestrogen, others include:
- Cereals – oats, barley, rye, brown rice, couscous, bulgar wheat
- Seeds – sunflower, sesame, pumpkin, poppy, flax, and linseed
- Pulses and beans – soya, chickpeas, kidney beans, haricot beans, broad beans, and green split peas
- Vegetables – red onions, celery, sweet peppers, garlic, broccoli, tomatoes, bean sprouts
Lifestyle changes
The good news is that there are immediate ways to tackle menopause symptoms through self-help lifestyle changes.
Diet
There isn’t one best menopause diet. But what we eat is central to how we feel and our general health.
Caffeine, alcohol, and spicy food can make hot flushes worse. Caffeine can also have a negative impact on your bladder. Some find the switch to decaffeinated tea and coffee makes a huge difference.
 The Mediterranean diet is associated with lower risks of heart disease (which can increase after menopause). A diet rich in calcium and vitamin D will help keep bones healthy as well.
The Mediterranean diet is associated with lower risks of heart disease (which can increase after menopause). A diet rich in calcium and vitamin D will help keep bones healthy as well.
Menopause can change the way your gut functions. To figure out which foods affect you, it can be a good idea to keep a diary. Bloating can be uncomfortable, so you may decide to avoid fizzy drinks, chewing gum, and gas-inducing foods including cabbage and sprouts (but make sure you’re still getting your five fruit and veg a day).
Many women drink alcohol in an attempt to help them through the menopause, especially to deal with sleep and anxiety. Although it may help you feel better at the time, it’s only temporary, as alcohol acts as a depressant on the brain. In the long run, cutting down can really help you feel better and support weight loss.
Weight gain is something that troubles lots of women, and losing weight can be a real challenge during the menopause. That’s because of changes to how your body handles carbohydrates and processes calories. Small changes to your diet can turn into dramatic and positive changes.
At My Menopause Centre, we can support you with diet and nutrition advice through our nutritionist partner.
Exercise
Even the smallest amount of exercise can have a positive impact on your health and wellbeing during the menopause . If you aren’t exercising regularly, then squeezing in a small amount is a start. No marathon running is required!
. If you aren’t exercising regularly, then squeezing in a small amount is a start. No marathon running is required!
Regular exercise helps mood and sleep (and even hot flushes for some). It can also help beat the weight gain often associated with menopause. Our friends at Her Spirit are well placed to help support and inspire you with exercise options.
One of the most important types of exercise for women during menopause is a regular weight-bearing or muscle-strengthening activity, like brisk walking or running. This will help to keep muscles and bones strong.
Stop smoking
If you smoke, we know you’ve heard it all before, but smoking really does worsen the effects of menopause. Smoking makes hot flushes worse[4] and increases your risk of cancer, heart disease, and osteoporosis. Quitting smoking will have a massive, positive impact on your journey through the menopause. The NHS stop smoking service can help you quit.
Other Therapies
Talking therapies and meditation
Yoga, meditation and mindfulness can help you deal with a frazzled mind. There are lots of apps and online resources for everyone, from novices to experts.
Cognitive behavioural therapy (CBT) involves talking about problems and finding ways to manage them by changing the way we process our thoughts. It takes practice, but it does work and comes recommended by the National Institute of Clinical Excellence.
There is great evidence to suggest that CBT helps menopause symptoms – and it’s a good skill to learn to help you to deal with a range of issues such as stress, anxiety, tiredness and pain, to name a few.
 We can help by offering CBT and counselling through experienced and highly qualified therapists, Sue and Claire.
We can help by offering CBT and counselling through experienced and highly qualified therapists, Sue and Claire.
We know many women find mindfulness a beneficial technique. It’s a way to exercise your attention and bring your focus to something positive so that the negative thoughts quieten.
Read our blog on our favourite meditation apps.
Coaching
Coaching can help you to appraise your life, make changes where needed and help you move forward positively while minimising stress. We have partnered with Kate Hesk and her team at Cognomie to support you in leading your best life.
Sex therapy
The menopause can significantly impact your sex drive and relationships. As well as HRT (including testosterone and vaginal oestrogens within this), you may need support in getting your relationship back on track.
We can help by offering sex and relationship counselling through an experienced and highly qualified sex therapist.
Physiotherapy
Many women suffer symptoms of prolapse and bladder issues. This isn’t confined to the menopause – some women experience it after having children, while some don’t experience it until later in life.
For those who haven’t come across the term, a prolapse is when the pelvic organs slip from their original positions because of weakness in the supports that hold them in place. The cervix and womb or bladder and bowel can bulge into the vagina.
Training the pelvic floor can help relieve the symptoms for some women. Others need treatment, such as a vaginal pessary or even surgery.
Physiotherapy can also help bladder symptoms, whether it’s stress incontinence or urgency of needing to go.
Chat through your options with an expert
As you can see, there are a wide range of options available to you to help relieve menopausal symptoms, and there certainly isn’t a one-size-fits-all approach. What’s most important is finding the right solutions for you and your situation, while weighing up the benefits and the risks. That’s where a chat with an expert can be worth its weight in gold.
To talk to a friendly and knowledgeable expert, and book a consultation with our menopause clinic.
Authored by:
Dr Clare Spencer
Registered menopause specialist, GP and co-founder; see Dr Clare in person at The Spire Hospital, Leeds or online
Last updated:
07/04/2021
Learn more
Join the pause. community
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Want to be the first to hear our latest news? Join our pause. community today.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Book a consultation
Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowReferences
-
Source: https://thebms.org.uk/wp-content/uploads/2018/03/Prescribable-alternatives-to-HRT-01EE.pdf
-
Source: Warren MP. Missed symptoms of menopause. Int J Clin Pract. 2007 Dec;61(12):2041-50. And NICE NG23 2015
-
Source: Prevalence of hot flushes and night sweats around the world: a systematic review. Freeman EW, Sherif K. Climacteric. 2007 Jun; 10(3):197-214.
-
Source: Ziv-Gal A, Smith RL, Gallicchio L, Miller SR, Zacur HA, Flaws JA. The Midlife Women’s Health Study – a study protocol of a longitudinal prospective study on predictors of menopausal hot flashes. Womens Midlife Health. 2017;3:4. Published 2017 Aug 17. doi:10.1186/s40695-017-0024-8.
Contact My Menopause Centre
- General enquiries: hello@mymenopausecentre.com
- Book appointments online: Log into your account and go to 'My appointments'
- Book appointments by phone: 0333 444 1067
- Website: https://www.mymenopausecentre.com


















