Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/knowledge/life-after-menopause/
Staying healthy in postmenopausal life
Menopause specialist Dr Clare Spencer explains how your postmenopausal body might continue to change as your hormone levels adjust to a new normal. Here's what to expect and advice on the things you can do to stay happy and healthy.
Explore

The term menopause refers to the day when your periods have stopped for 12 months (because your ovaries aren’t making hormones), marking the end of fertility. The average age of the menopause in the UK is 51. Around 5% of women will go through an early menopause, between the age of 40-45, and 1% under the age of 40. This is known as Premature Ovarian Insufficiency, or POI.
As soon as you have been through the menopause you immediately become postmenopausal and you’re postmenopausal for the rest of your life.
A new second act
In previous generations, women experienced the menopause later and didn’t live as long as we do today:
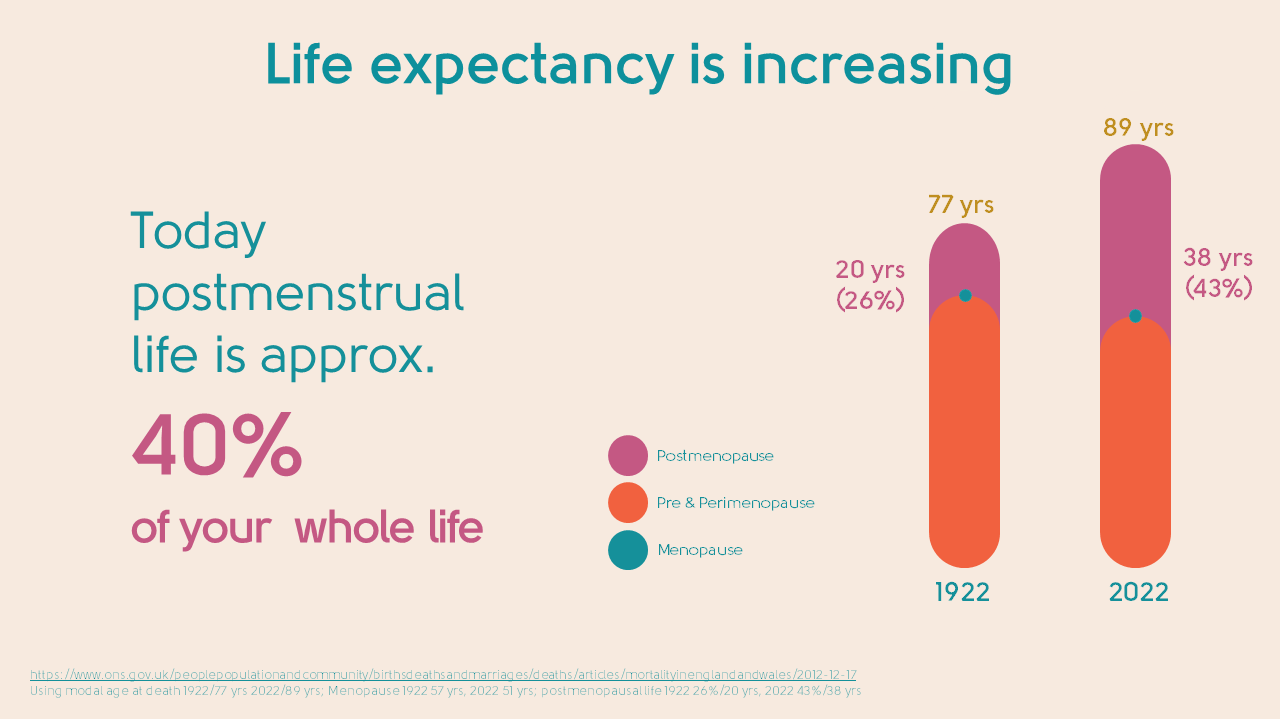
In 1922, the modal age of death for a woman was 77[1] and the average age for going through the menopause was 57. One hundred years later, life expectancy for a woman has increased to 89 years[2] and the average age of menopause has fallen to 51. So this means she could spend at least 40% of her life postmenopausal – that’s a whopping 38 years! Every woman is entitled to enjoy this time feeling as healthy, happy, and vibrant as possible.
Menopause presents us with an opportunity to take stock of our lives – our physical and mental wellbeing, our happiness, and our priorities – and create a plan for a great second act.
Many women find being free from periods liberating and, as their symptoms start to improve, they rediscover a zest for life.
A good time to reflect on your health
In the postmenopause, oestrogen levels are low and stay low. Most oestrogen is made by your ovaries. You can see how this differs from our premenopausal stage in the illustration below.
- Before the menopause transition (perimenopause), oestrogen levels generally fluctuate during a monthly cycle.
- Levels change wildly and unpredictably during the perimenopause.
- And then levels drop and stay low in the menopause and postmenopause.
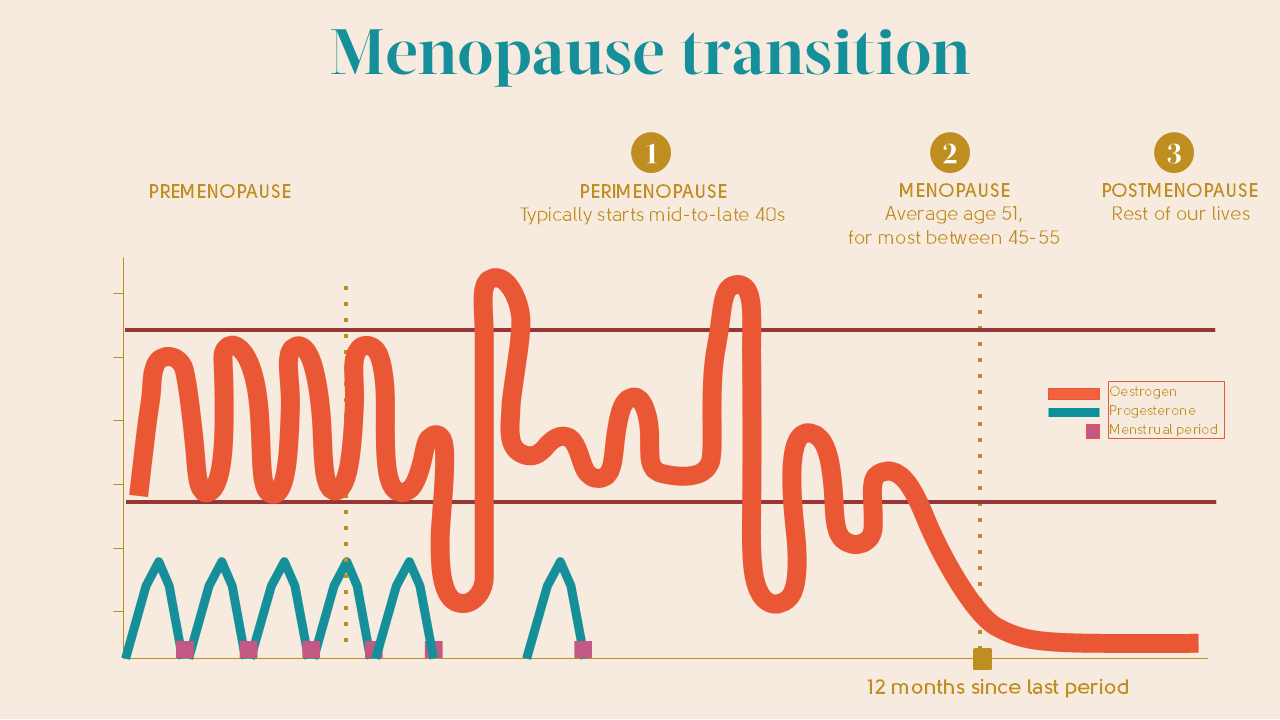
It’s the fluctuation in, and then drop of, oestrogen that is responsible for most menopause symptoms. As well as causing these symptoms, low oestrogen levels can have a significant impact on our bodies. They can increase the risk of osteoporosis and heart disease and are also responsible for changes to the tissue of the vagina and bladder that can continue to worsen in the postmenopause. For some, there are changes to mood too.
With these risks in mind, the menopause is an important time to take stock of your health and see what you can do to reduce the risk of osteoporosis and heart disease in particular.
Looking after your heart health
Before the menopause, the risk of heart disease for women is lower than that of men. The risk of heart disease increases after the menopause, and an important contributory factor to this is the loss of oestrogen postmenopause. You may not realise that twice as many women die from heart disease than from breast cancer[4].
Oestrogen has a protective effect on the heart and it’s the loss of oestrogen that contributes to changes that increase the risk of heart disease. Hormone Replacement Therapy (HRT), if started within 10 years of the menopause (or under the age of 60), can go some way to reducing the risk, but lifestyle factors are also really important: smoking, high alcohol intake, being overweight and lack of physical activity.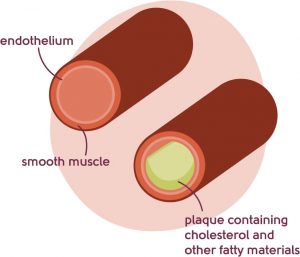
Other important factors for heart disease include high blood pressure, diabetes, high cholesterol, and for some, a family history of heart disease or other medical conditions.
As you can see, this list includes some risk factors that are in your control. The menopause is a good time to consider making healthy adjustments to your lifestyle – we’re not saying it’s easy, but there’s lots of support available to help you.
Monitoring your diet to maintain a healthy weight can help cholesterol, diabetes and ultimately, the risk of heart disease. Regular exercise is likewise a great way to help reduce the risk of heart disease.
You can find out more about heart disease in the menopause here.
If you’re worried about your risk of heart disease, please speak to your doctor. They can check your cholesterol level and blood pressure and talk to you about your lifestyle.
Osteoporosis – look after your bones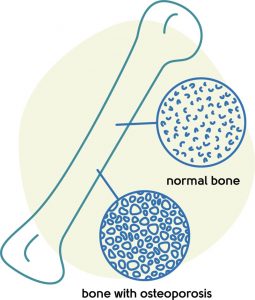
Osteoporosis is a condition where bones become weaker, less dense and more prone to breaking.
Oestrogen is important for maintaining bone mass, and in the illustration of oestrogen levels above, you can see how these fall in the menopause. Osteoporosis is an age-related condition that results in reduced bone mass and increased susceptibility to bone fracture.
The risk increases with age and the menopause has an impact. A woman can lose up to 20% of her bone density during the five to seven years following the menopause[5], but like heart disease, the menopause not the only risk factor.
Others include smoking, drinking too much alcohol, being underweight, having a family history of osteoporosis, malabsorption conditions, certain medical conditions and being on certain medication.
There are risk factors on this list that are in your control, and it’s yet another reason to take regular exercise. This is because weight-bearing exercise can help reduce your risk of osteoporosis, high blood pressure and heart disease.
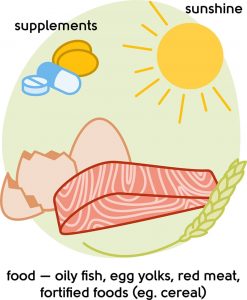
Making sure you are getting enough vitamin D and calcium can also help reduce the risk of osteoporosis (see illustration for sources of vitamin D and calcium).
HRT, although prescribed for symptom control, can also be beneficial. You can find out more about osteoporosis here.
Bladder issues
The loss of oestrogen during the menopause transition makes the tissue of your bladder more sensitive and delicate. Instead of happily expanding as it fills with urine – like filling a balloon with water – the bladder gets irritated and starts to squeeze to empty before it should do. This can lead to discomfort and pain. Bladder symptoms become more likely as you get older, as the effects of lack of oestrogen on the bladder take their toll. 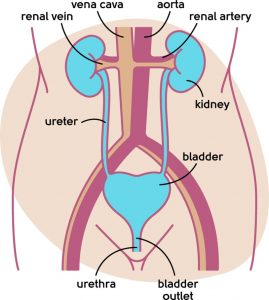
These symptoms sometimes stop some women from exercising because they’re afraid of leakage, and can prevent others from leaving the house, or joining in social events. It doesn’t have to be like this though. These symptoms are remarkably common and your doctor will not be embarrassed, so you don’t need to be either. If you need help, just ask.
You can find out more about bladder issues (and ways to treat them) here.
Vaginal symptoms
Vaginal symptoms become increasingly common as you age. Approximately two-thirds of postmenopausal women who haven’t taken HRT suffer from changes in the vagina and bladder linked to low oestrogen. These symptoms can have a knock-on effect on sex and relationships. So our message here is that you don’t have to just put up with it – because, for most women, these symptoms are easy to treat.
You can read more about the loss of sex drive here.
Perhaps just as important as these, are the emotional and psychological tools that a psychosexual therapist can give you – read more by Sue Makin, our psychosexual therapist on our blog or view her partner page.
Make the most of screening
To give yourself the best possible chance of a long and healthy postmenopausal life, we urge you to attend regular cervical smears and mammograms in line with UK screening programmes. However busy you are, don’t let day-to-day life get in the way of doing all you can to protect yourself against cancer.
Taking HRT over 60
There’s no right answer to the question about how long to take HRT for, and there’s no arbitrary age cut-off. The benefits and risks will differ for every woman as they enter their 60s (and beyond).
HRT is effective in treating menopause symptoms – important when around 5% of women continue to experience symptoms of the menopause for 15 years and longer[6].
The main risks of using HRT to consider are the increased risk of breast cancer and, with oral HRT, the increased risk of blood clots and stroke.
The risk of breast cancer increases with age and with the length of time you take HRT [7]. The baseline risk of blood clots and stroke also increases with age. Oral HRT significantly increases the risk of blood clots and stroke, whereas HRT forms where the oestrogen is given through the skin (like patches, gels and sprays) does not further increase the age-related risk. Furthermore, the dose of oestrogen that you are likely to need decreases with age.
As with heart disease and osteoporosis, there are ways of managing these risks that are in your control: monitoring your diet to maintain a healthy weight, moderating your alcohol intake, and quitting smoking. Regular exercise can also reduce the risk [8].
The benefits and risks of HRT will differ for every woman, so our advice would be to discuss the ongoing use of HRT with your doctor. You don’t have to stop it just because you are 60 or older, but you do need to understand how the benefits and risks of HRT apply to you.
There’s lots of detailed information about HRT on our HRT resource page and in our FAQs.
Your mind and mental health
More than half of women suffer from postmenopausal mood changes[10]. It’s not just ‘one of those things’. It’s important and it’s vital that you talk about it.

Women’s mood can improve after the menopause[11]. This is more likely to happen when they find more time for themselves, pursue new interests, or rediscover old ones that got lost in the whirlwind of child-rearing, relationships, and all the responsibilities of life. Developing a more positive view of the menopause can make it much easier to come through it smiling.
But all of this doesn’t take anything away from the fact that this is a tricky time of life, even without the menopause. Maybe your children are leaving home, or you have caring responsibilities, perhaps you have medical issues of your own, or maybe you have ended a long-term relationship.
So give yourself a break. Try to find pockets of time that are just about you and focus on all the positives that are yet to come – there are plenty.
If your mood changes are related to the menopause, evidence suggests that HRT is better at improving your mood than antidepressants[11]. It may be worth a try, even for a short period, to see if it helps.
Empty nest syndrome
This is a phrase used to describe that time when children (if you’ve had them) start to leave for university or move in with friends and partners of their own. It’s traditionally seen as a negative thing, but the lives of women today are different from those of previous generations. We’re much more likely to be working outside of the home, with responsibilities and friends to keep us stimulated. Don’t forget, this isn’t necessarily just a time for endings.
You may decide to take up a new job, retrain or start that business you’ve always dreamed of. Maybe you’re beginning a new relationship with all the excitement and possibility that brings. You could still be raising teenagers or looking after grandchildren.
More frequently, women are finding that their 20-something children are still living at home while they try to get the finances together to rent or buy their own place. Plus, technology and social media have made keeping in touch with a wide circle of friends and far-flung family members easier than ever. We’re connected like never before. So those ‘empty nests’ aren’t necessarily all that empty.
 We appreciate everyone has different home and lifestyle situations. You don’t have to have had children to feel alone during the menopause. If you’d like to share your story or hear from other women, you can sign up to be part of our pause. community.
We appreciate everyone has different home and lifestyle situations. You don’t have to have had children to feel alone during the menopause. If you’d like to share your story or hear from other women, you can sign up to be part of our pause. community.
We recommend focusing on the positives, the opportunities, and the ways you can continue to grow, evolve, and thrive. This isn’t an end, it’s the beginning of a second act.
Our top tips for living your healthiest postmenopausal life
- Take stock and take control of any lingering menopause symptoms and commit to taking action. Speak to your GP or one of the doctors in our menopause clinic about what you can do to treat them. It’s never too late to have the discussion.
- Look at your lifestyle. Start exercising regularly, develop healthy eating habits and ensure you’re getting enough sleep at night.
- Go for regular health screenings.
Always remember our mantra – knowledge is power. So take the time to understand your body, to understand the menopause – and to take control. We’re with you all the way.
What next?
Hopefully, you now understand a little more about postmenopause life and what to expect from it. Many women find our Menopause Questionnaire helps them understand if they are postmenopausal or not.
You can use our symptom checker to see if you still have symptoms. Or perhaps you’d like to book an appointment with our menopause clinic to speak to one of our highly experienced doctors.
Last updated:
07/04/2021
Related pages
Join the pause. community
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Want to be the first to hear our latest news? Join our pause. community today.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Book a consultation
Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowReferences
-
Source: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/mortalityinenglandandwales/2012-12-17
-
Source: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/mortalityinenglandandwales/2012-12-17
-
Gartoulla P, Worsley R, Bell RJ, Davis SR. Moderate to severe vasomotor and sexual symptoms remain problematic for women aged 60 to 65 years. Menopause. 2018 Nov;25(11):1331-1338.
-
https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/women/coronary-heart-disease-kills accessed March 2021
-
Ballard, P., Purdie, D., Langton, C. et al. Prevalence of Osteoporosis and Related Risk Factors in UK Women in the Seventh Decade: Osteoporosis Case Finding by Clinical Referral Criteria or Predictive Model? . Osteoporos Int 8, 535–539 (1998).
-
Gartoulla P, Worsley R, Bell RJ, Davis SR. Moderate to severe vasomotor and sexual symptoms remain problematic for women aged 60 to 65 years. Menopause. 2018 Nov;25(11):1331-1338.
-
Collaborative Group on Hormonal Factors in Breast Cancer. Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Lancet. 2019 Sep 28;394(10204):1159-1168.
-
Parkin, DM, Boyd, L, Walker, LC. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br J Cancer 2011; 105: S77–S81.
-
Vinogradova Y, Coupland C, Hippisley-Cox J. Use of hormone replacement therapy and risk of venous thromboembolism: nested case-control studies using the QResearch and CPRD databases. BMJ. 2019 Jan 9;364
-
Currie H, Moger SJ. Menopause – Understanding the impact on women and their partners. Post Reprod Health. 2019 Dec;25(4):183-190.
-
Leonhardt M. Low mood and depressive symptoms during perimenopause – Should General Practitioners prescribe hormone replacement therapy or antidepressants as the first-line treatment? Post Reprod Health. 2019 Sep;25(3):124-130.
Contact My Menopause Centre
- General enquiries: hello@mymenopausecentre.com
- Book appointments online: Log into your account and go to 'My appointments'
- Book appointments by phone: 0333 444 1067
- Website: https://www.mymenopausecentre.com


















