Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/knowledge/menopause-explained/
Understanding Menopause
Our co-founder and registered menopause specialist, Dr Clare Spencer, explains what the menopause is, the stages of menopause transition, what to expect in each (including when it starts, duration and symptoms), and treatment options.
Explore
What is the menopause?
The menopause is a completely normal and natural part of a woman’s life. It’s a time when our hormones are changing, and our bodies are shifting towards the end of fertility. It’s a period of our lives to take stock and look after ourselves so that we can live our best lives and thrive going forward.
The word ‘menopause’ literally means the ‘end of monthly cycles’ (the end of monthly periods or menstruation), from the Greek word pausis (‘pause’) and mēn (‘month’).
The menopause explained
Let’s start with a short summary of what’s going on in our bodies before the menopause begins.
During our reproductive life, every month an egg is released from our ovaries which also rhythmically releases hormones (chemical messengers), namely oestrogens, progestogens and androgens.
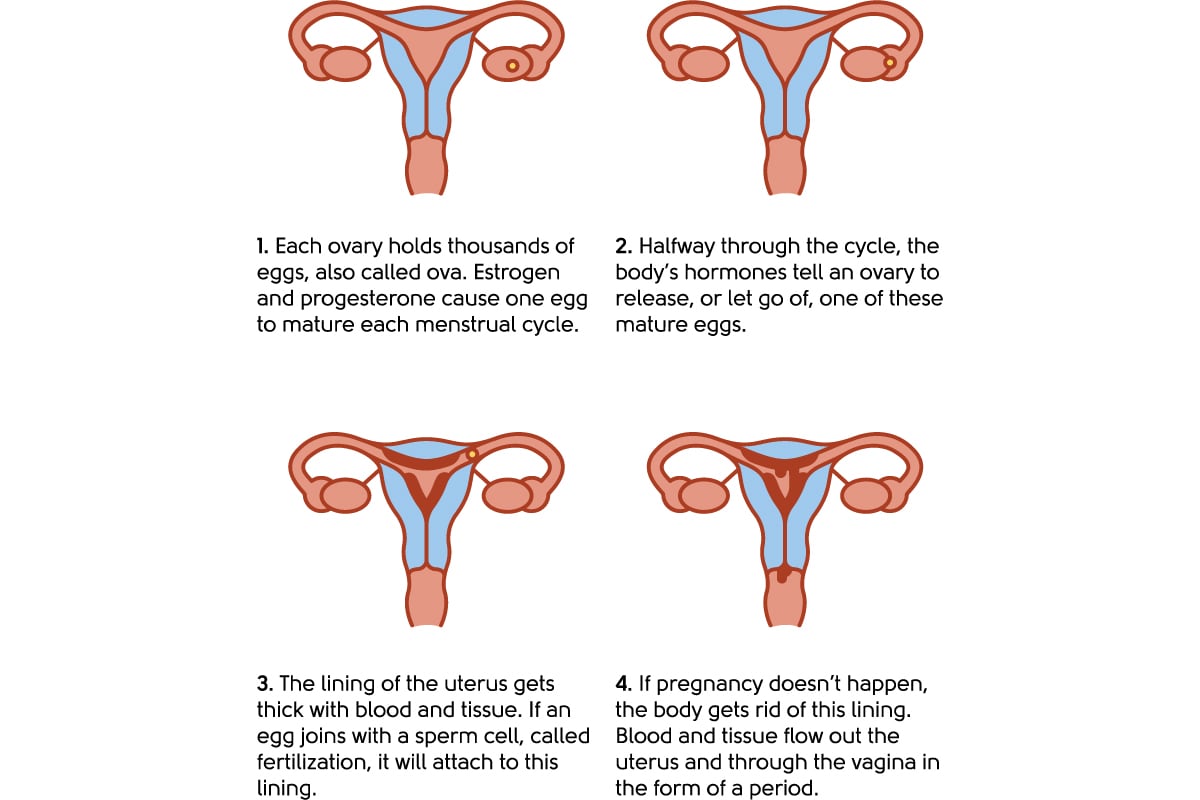
Illustration to show the menstrual cycle
Meanwhile, our brains make hormones called follicle-stimulating hormone (FSH) and luteinising hormone (LH), which are essential for communication between the brain and the ovaries. Hormones relay messages from the brain to the ovaries and back again to keep everything running like clockwork.
When we start to run out of eggs, our ovaries begin to produce fewer hormones, particularly oestrogen, and the levels can fluctuate wildly. Our brains make more FSH to try to balance things out when oestrogen levels are low. The changing levels of hormones from the ovaries give many of us symptoms – some of which are well known (hot flushes) and some less so (joint pains). This stage of the menopause transition is known as the perimenopause.
You can find out more about menopause symptoms here.
The menopause occurs when your ovaries permanently stop producing eggs. Your oestrogen levels are now always low, and your FSH levels are permanently high. If you have a blood test to see if you’ve reached menopause, your doctor will check the FSH and, sometimes, oestrogen levels.
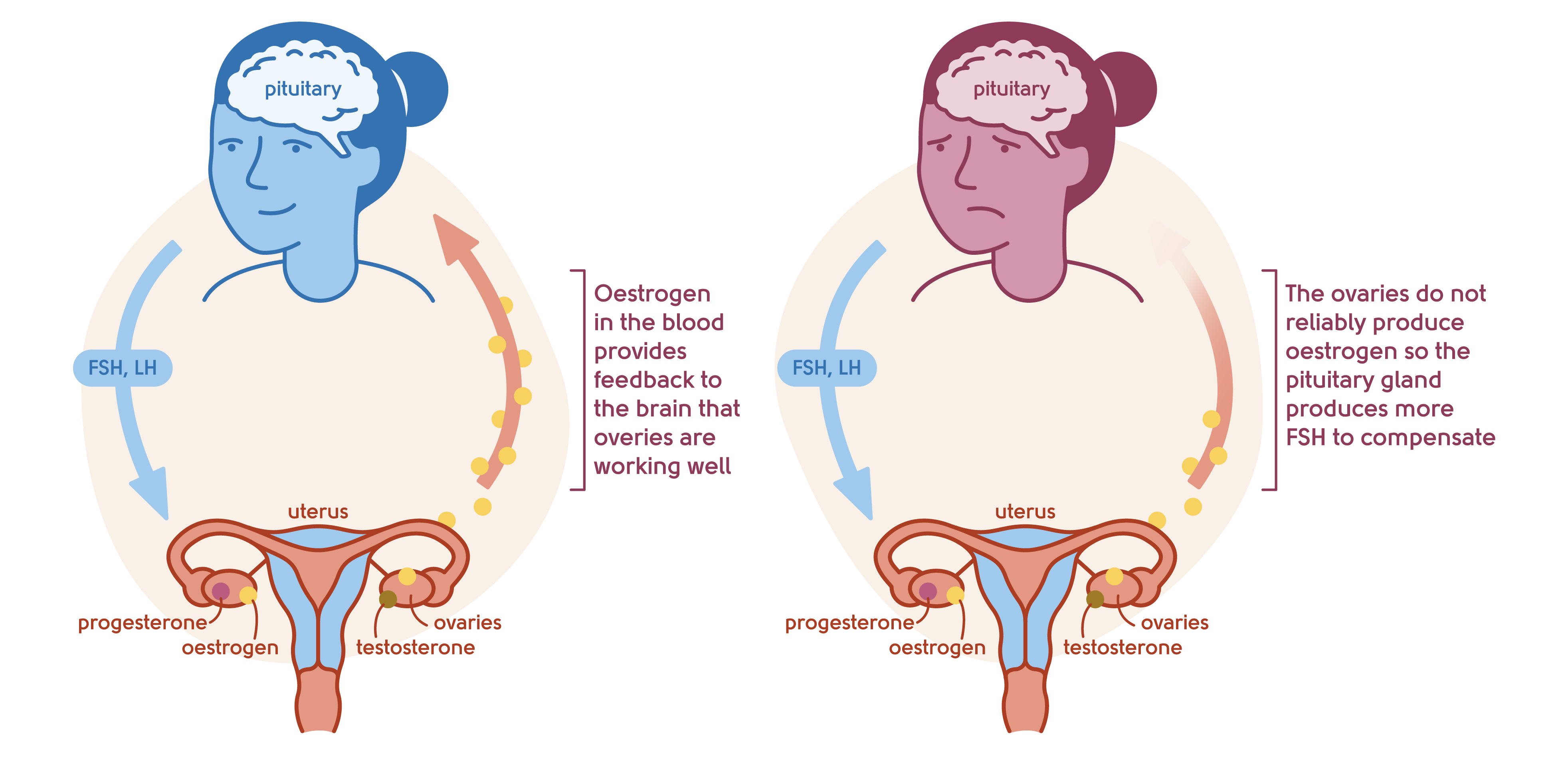
Illustration to show the feedback mechanism of the ovaries and the brain
What do the terms ‘surgical’ and ‘medical’ menopause mean?
Some women enter menopause for reasons other than natural changes in their hormones. The two most common types are surgical and medical menopause:
Surgical menopause – this occurs when a woman’s ovaries are removed. Hormone levels plummet, and she immediately experiences menopause.
Medical menopause – this occurs when a woman’s ovaries stop working due to chemotherapy, other medicines, or radiotherapy.
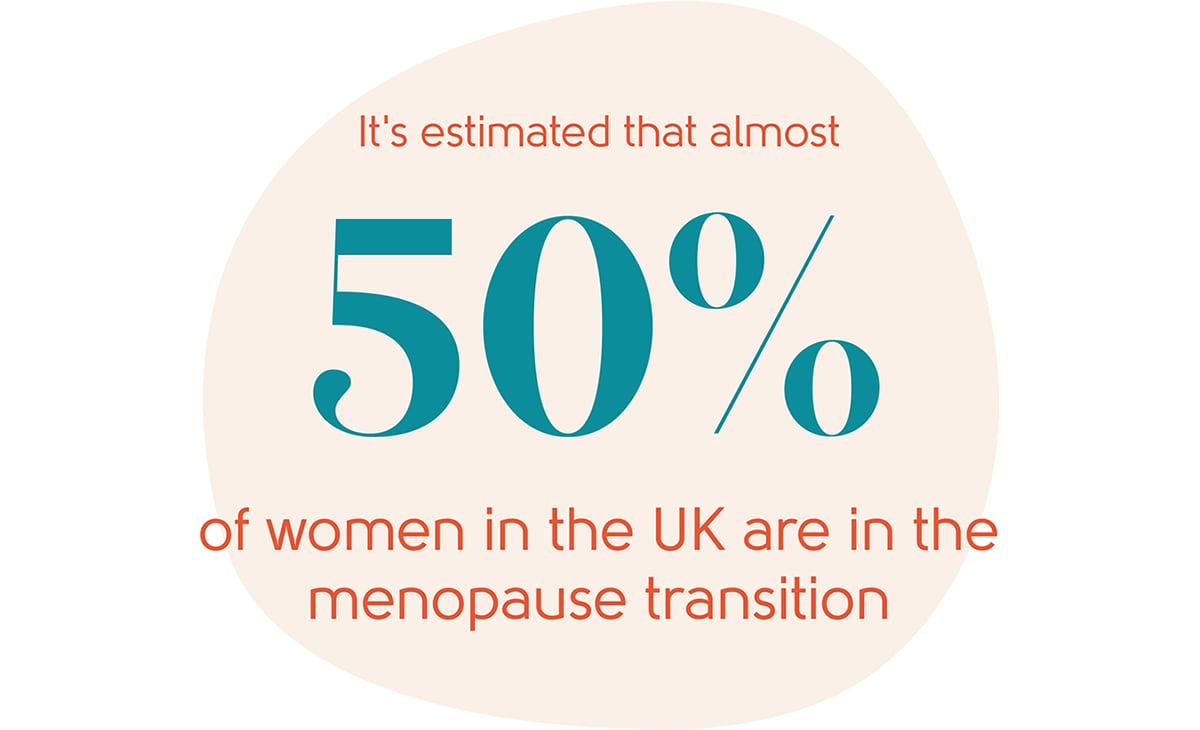
There are an estimated 15.5m women in the UK today who are at some stage of the menopause transition (perimenopause, menopause, and postmenopause). Each of these stages is explained in more detail below.
What are the different stages of the menopause transition?
There are three stages to the menopause transition:
- Perimenopause
- Menopause
- Postmenopause
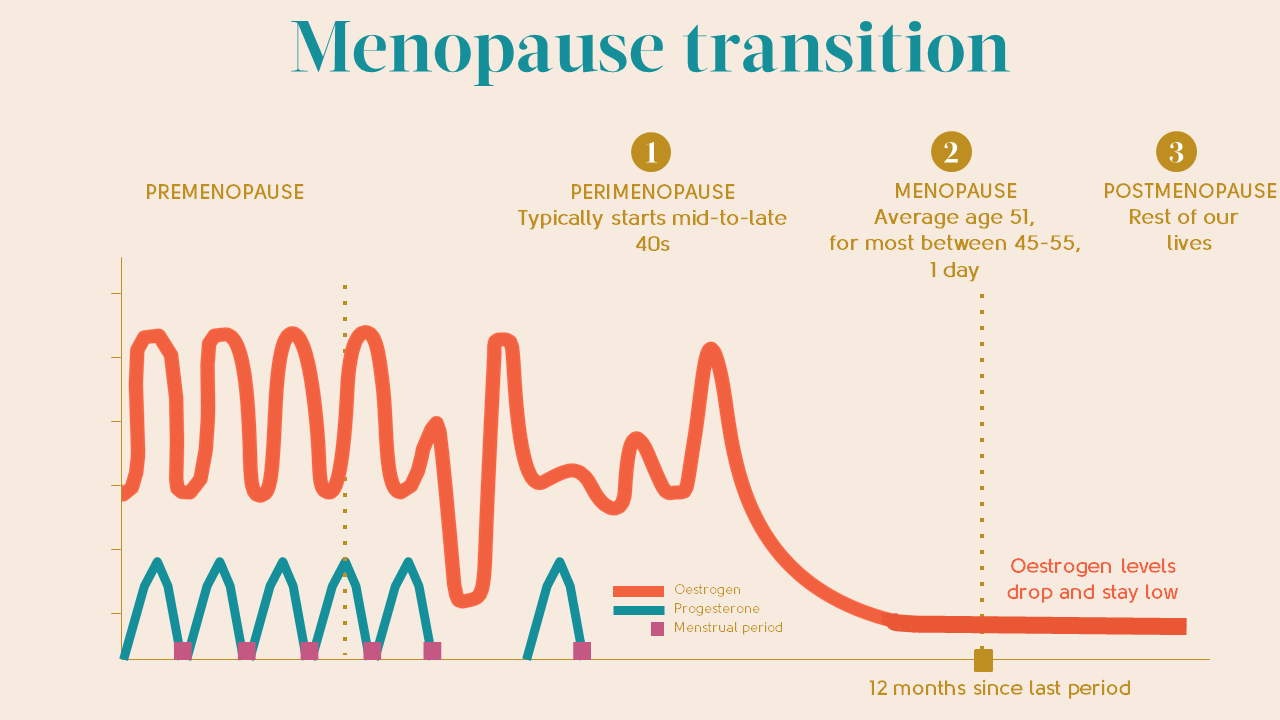
The menopause transition usually starts when a woman is in her mid-to-late 40s (known as the perimenopause) but it’s important to be aware that some women will start the menopause transition at a younger age than this and some at an older age. The average age for a woman to reach the menopause in the UK is 51. Around 5% of women will go through an early menopause, between the age of 40-45, and 1%under the age of 40. This is known as Premature Ovarian Insufficiency, or POI.
8 in 10 women experience symptoms of the menopause, and the duration of these symptoms can vary greatly. For most women symptoms last around eight years, but can be shorter for some women and longer for others – it’s different for everybody.
I’ve clearly seen that every single woman is different in her experience – in the range of symptoms, how severe they are, how long they last, and the impact they have. It’s why care is not one size fits all. Personal, tailored care is a must.
Dr Clare Spencer, Co-Founder of My Menopause Centre
Perimenopause
The perimenopause is the time leading up to the menopause when your ovaries start to run out of eggs. This means hormone production decreases and, as a consequence, periods can be irregular, less frequent, heavier or lighter, and generally unpredictable. Although for some women, periods don’t change.
You may also experience symptoms during perimenopause as hormone levels can be all over the place and generally drop.
Many women don’t realise they are in the perimenopause because menopause symptoms can creep up on them. They may be subtle, such as feeling a little more anxious, or mood swings can dip lower than usual. Symptoms can come and go and change in intensity. Symptoms may be also associated with other medical conditions or just put down to ‘ageing’ rather than being recognised as being due to the menopause.
You can find out more about menopause symptoms here.
The perimenopause typically starts in your mid-to-late 40s but for some it can be earlier or later.
Menopause
The menopause is said to occur after 12 consecutive months of no bleeding because your ovaries have stopped producing hormones (that is, there is no other obvious cause for your periods to have stopped such as pregnancy, breastfeeding, or taking hormonal contraception).
You’re menopausal literally for a day, and after that you’re postmenopausal.
The average age of the menopause in the UK is 51 and for most women, their periods have naturally stopped by the age of 55.
Postmenopause
As soon as you have been through the menopause, you immediately become postmenopausal and you’re postmenopausal for the rest of your life. In this third phase of the menopause transition, you may still experience symptoms, commonly for a further five to seven years, though many experience symptoms for longer than this.
You can learn more about staying healthy in postmenopausal life here.
What is premature menopause or Premature Ovarian Insufficiency (POI)?
Premature menopause or Premature Ovarian Insufficiency (POI) occurs when a woman experiences the menopause under the age of 40. This occurs in 1% of women[1] and can be a devastating diagnosis.
If you are worried that you may be becoming menopausal under 40, it’s essential to speak to your doctor about it as they can arrange tests and give you the support you need.
It is so important that you get the correct advice about HRT to replace the oestrogen that your body is no longer producing. This can help with symptoms and, significantly, help prevent long-term health risks. A GP can refer you to the fertility clinic for a review and to discuss options if you wish to have children.
Early menopause happens between 40-45 years of age and is experienced by an estimated 5% of women.[2]
How long does the menopause last?
It’s different for every woman.
The perimenopause stage of the menopause transition lasts a variable length of time, typically five years but it can be up to eight to ten years.
The menopause itself lasts a day and then you’re postmenopausal for the rest of your life.
Symptoms can continue in the postmenopause too, on average for around five to seven years. Take hot flushes for example: while women can experience these, on average, for about seven years, over 40% of women aged between 60-65 years will continue to experience hot flushes and night sweats[3] and some will experience them for up to 20 years following menopause.
I have women in my clinic in their 70s and 80s still experiencing hot flushes.
Dr Clare Spencer, Co-Founder of My Menopause Centre
What if I am not having regular periods because of contraception?
If you don’t have a period because you’re taking hormones (like a Mirena™ coil or contraceptive hormone tablets), it can be difficult to tell if you’re transitioning through the menopause and if so, what stage you’re in, because we don’t know if your ovaries are still producing hormones. You can’t tell if you would have been having periods or not if you weren’t using that particular type of contraceptive.
Keeping an eye on your symptoms – or lack of them – is often the best way to tell if you’re experiencing menopause or not.
As a side note, a Mirena™ coil can be a useful part of HRT. We recommend that you don’t rush to remove it if it’s not causing issues and it’s less than five years old.
What if I have had a hysterectomy?
Many women ask if having a hysterectomy means they are in the menopause. If you’ve had a hysterectomy – that is, if you have had your womb removed but you still have your ovaries – your periods will stop as period blood comes from your womb.
Your ovaries will carry on as normal, producing hormones for as long as they were programmed to. You won’t know when your last period was meant to be – but this doesn’t matter in terms of treatment options. What matters most is your symptoms and how you feel.
On average, women who have had a hysterectomy before the menopause may have an earlier menopause than if they hadn’t had a hysterectomy.
How does menopause affect fertility?
Fertility starts to decline from the mid-30s, particularly after the age of 35. Women’s fertility keeps decreasing every year and continues to drop in the perimenopause.
Just because you’re reaching menopause doesn’t mean you don’t have to think about contraception. If you have unprotected sex over the course of the year and you are aged 40-44, the chance of pregnancy is around one in five, and this drops to about one in 10 from age 45-49. So you do still need to use contraception if you don’t want to get pregnant.
It’s rare (but not impossible) to get pregnant over the age of 50 and you can stop using contraception once you’re 55.
Is a blood test useful?
FSH and oestrogen can be measured in the blood, so a blood test can be useful in finding out if your periods have stopped because of menopause, particularly if you’re under 40.
The thing to remember when we’re talking about measuring FSH in perimenopause is that levels in your body can change day-to-day. So it’s not a very reliable way of finding out if your periods have stopped, or are likely to stop soon.
If you have symptoms, your periods have stopped and you’re over 45, checking your FSH level won’t make any difference to your options for managing your symptoms. Nor will it tell you anything useful (like how long symptoms will last or how severe they will be).
There is a role for a blood test, though. Measuring FSH levels can be useful if your periods have stopped because of your contraception. If you’re using hormone contraception that stops periods (like the Mirena™ coil or mini pill), a high FSH level can help your doctor work out when you can stop using contraception.
You can read more about blood testing for oestrogen levels here.
Thriving through the menopause
Did you know that women today can expect to live over 40% of our lives after going through the menopause?[4] What better reason to take care of your menopause symptoms and long-term health – make the most of your second act in life and live it to the full!
Find out more about staying healthy in postmenopausal life here and read more about different ways to treat your menopause symptoms here.
What next
Hopefully, you now understand a little more about the menopause. You can read more about the symptoms of the menopause and the different treatment options in Menopause Explained. Many women find our Menopause Questionnaire helps them understand if they are going through the menopause transition or not.
If you’d like to speak to one of our experienced doctors about your symptoms, you can book an appointment with our online menopause clinic here.
Authored by:
Dr Clare Spencer
Registered menopause specialist, GP and co-founder; see Dr Clare in person at The Spire Hospital, Leeds or online
Last updated:
07/04/2021
Learn more
Join the pause. community
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Want to be the first to hear our latest news? Join our pause. community today.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Book a consultation
Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowReferences
-
Source: Luborsky JL, Meyer P, Sowers MF, Gold EB, Santoro N. Premature menopause in a multi-ethnic population study of the menopause transition. Hum Reprod 2003;18: 199-206.
-
Source: Shifren, J.L., Gass, M.L.S., for the NAMS Recommendations for Clinical Care of Midlife Women Working Group. (2014). The North American Menopause Society Recommendations for Clinical Care of Midlife Women. Menopause; 21(10): 1038–1062.
-
Source: Shifren, J.L., Gass, M.L.S., for the NAMS Recommendations for Clinical Care of Midlife Women Working Group. (2014).
-
Source: https://www.ons.gov.uk/
Contact My Menopause Centre
- General enquiries: hello@mymenopausecentre.com
- Book appointments online: Log into your account and go to 'My appointments'
- Book appointments by phone: 0333 444 1067
- Website: https://www.mymenopausecentre.com


















