Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/symptoms/osteoporosis/
Menopause and osteoporosis
Osteoprosis is a condition where bones lose density, a change directly linked to a loss of oestrogen. There are no symptoms unless bones break.
Explore
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentIf you would like to learn more about the impact of your symptom(s) complete our free online menopause questionnaire here.
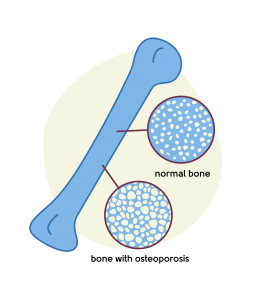
What is osteoporosis?
You’ve probably not given much thought to bone health before, but it’s an important topic – especially at this time in our lives. Osteoporosis is a condition where the bones become weaker, less dense, and more prone to breaking.
Osteoporosis becomes more common as we go through the menopause, and at the age of 50, around 2% of women have osteoporosis. This goes up to 25% by the time we are 70 years old[1].
The risk of developing osteoporosis is greater for women who have Premature Ovarian Insufficiency (POI). If this is you, and you haven’t already done so, it’s really important to talk to your doctor about taking HRT to prevent osteoporosis. See below for more on HRT.
Osteoporosis develops slowly, usually over years, and you probably won’t know it’s happening to you until you break a bone, more often than not as a result of a low-impact injury.
Small fractures of the spine lead to pain and a change in posture and height. Osteoporosis is much more common in women than in men.
It’s important to think about the prevention and treatment of osteoporosis in our younger years – our 30s, 40s, and 50s – to help prevent fractures as we grow older.
To diagnose osteoporosis, you need a scan called a DEXA scan. This is a bone density scan that uses low-dose X-rays to see how dense (or strong) your bones are.
A DEXA scan may also diagnose osteopenia, a condition where the bones are ‘thinner’ or less dense than normal, but not as brittle as in osteoporosis. Osteopenia can get better (as can osteoporosis) and having this diagnosis does not mean that you will develop osteoporosis.
What causes osteoporosis?
There are many risk factors for osteoporosis in the menopause transition. Low(er) levels of oestrogen, calcium and vitamin D are all important factors, although they’re not the only ones. Other hormones, such as progesterone and testosterone, have a role to play, as does your diet.
Oestrogen is a hormone that’s important for bone health. Our bones are constantly being renewed, so there’s destruction and rebuilding of bone all the time. Oestrogen is important in the rebuilding part. The loss of oestrogen in the menopause can result in less renewal, resulting in ‘thinner’ or less dense bones that are more prone to fracture.
Calcium is a ‘building block’ that’s stored in our bones. It’s essential for maintaining bone mass. Vitamin D is also needed so that we can absorb the calcium from what we eat. If you have a low vitamin D level, it means you can’t absorb as much calcium.
There are other important risk factors for osteoporosis apart from the menopause. These include:
- Low body weight
- Drinking too much alcohol
- Smoking
- Your genes
- Increasing age
- A history of broken bones
- Medication
- Other medical conditions:
- Rheumatoid arthritis
- Excessive exercise
- Anorexia
- An over-active thyroid gland
- Conditions that affect how well the gut can absorb food
- Conditions where there are long periods of immobility
- Diseases of the parathyroid gland
- Conditions where there are lower levels of oestrogen or (particularly for men) testosterone
How many women typically experience osteoporosis?
About 1 in 3 women and 1 in 5 men will suffer from a bone fracture as a result of osteoporosis in their lifetime. Women aged over 45 years spend more days in hospital because of osteoporosis than diabetes, heart attack or breast cancer.[2]
Is osteoporosis linked to any particular stage of the menopause?
The risk of osteoporosis increases with age. Osteoporosis that’s a result of the menopause (that is, it’s not because of another disease process) is more common 10 to 15 years after the menopause[3].
For some women, bone loss happens faster than for others. In fact, a woman can lose up to 20% of her bone density during the 5-7 years following the menopause. If you lose bone density quickly, you have a greater chance of developing osteoporosis[4].
How can osteoporosis be treated?
Thankfully, there’s a range of things you can do to keep your bones healthy and reduce the risks of osteoporosis. You don’t need to accept it as an inevitable result of ageing.
Hormone Replacement Therapy (HRT)
Numerous studies have confirmed the beneficial effect of HRT on the skeleton, and shown that it reduces the number of broken bones and can prevent bone loss[5].
Women who have had an earlier menopause transition are at greater risk of osteoporosis. This is why women who have gone through menopause under the age of 40 should discuss HRT with their doctor.
You may feel anxious about taking HRT because of the well-publicised small risks, particularly of breast cancer. In reality, these risks are tiny for most women. Lifestyle factors, such as how much you weigh and how much alcohol you drink, can have a greater impact on your risk of breast cancer than HRT.
For most women, the benefits of menopause symptom control and the reduction in the risk of osteoporosis and heart disease far outweigh any small risks.
You can find out more about HRT here.
Calcium and vitamin D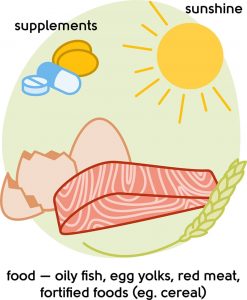
It’s important to make sure you have enough of both. Vitamin D is made by the body in response to sunlight on the skin. It’s also found in certain foods, such as fish, eggs and fortified food such as bread and cereal.
Vitamin D is needed to absorb calcium in the gut and it helps regulate the amount of calcium and phosphate in the body.
Calcium is found in dairy products, tofu, nuts, and leafy green vegetables. The recommended daily intake of calcium for women is 700mg, which is the equivalent of a pint of semi-skimmed milk.
You might consider taking calcium and vitamin D supplements if you don’t eat these types of food. During the spring and summer (late March/early April to the end of September) the sunlight is sufficient to help our bodies make enough vitamin D, though you may want to consider taking a supplement if you work indoors all day.
It’s recommended to take a vitamin D supplement containing at least 10 micrograms (400 international units IU) of vitamin D during the autumn and winter.
If you’re at risk of having low vitamin D, the recommendation is a daily supplement containing 10 micrograms of vitamin D throughout the year.
Regular exercise
The most useful exercises are weight-bearing and resistance. Weight-bearing exercises are where the weight goes through your feet and legs – for example, brisk walking, running, and aerobics.
Resistance exercises are where you move your body, a weight, or some other form of resistance against gravity – for example, free weights, resistance bands, or using your body weight to do squats or warrior poses.
Our friends at Her Spirit have lots of help and advice available. They can help you find an activity for you and provide the support to do it.
 Stop smoking
Stop smoking
As well as reducing your risk of smoking-related bone loss, it will also reduce your risk of cancer. If you would like help to quit, the NHS is a great place to start.
Drink less alcohol
Many women turn to alcohol during the menopause to get through their symptoms. Cutting out or cutting down on your intake can help your bone-building, as well as the absorption of vitamin D and calcium.
Management and treatment
If you’re diagnosed with osteopenia, you should have a good look at your diet, exercise, and lifestyle. Making changes now can prevent you from progressing to osteoporosis. Speak to your doctor about ways of managing it.
If you’re diagnosed with osteoporosis, your doctor will talk through the available treatments to treat osteoporosis and whether you need treatment to prevent fractures in the future, depending on your other risk factors.
What next?
If you’re concerned about bone health and osteoporosis, see your GP or book an appointment with our menopause clinic.
If you think you may be experiencing symptoms of the menopause transition, you can learn more with our symptom checker or by taking our Menopause Questionnaire.
You can also find more information about the menopause transition at the British Menopause Society and the National Institute for Health and Care Excellence.
Authored by:
Dr Clare Spencer
Registered menopause specialist, GP and co-founder; see Dr Clare in person at The Spire Hospital, Leeds or online
Last updated:
07/04/2021
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentLearn more
Join the pause. community
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Want to be the first to hear our latest news? Join our pause. community today.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Book a consultation
Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowReferences
-
Source: Ballard, P., Purdie, D., Langton, C. et al. Prevalence of Osteoporosis and Related Risk Factors in UK Women in the Seventh Decade: Osteoporosis Case Finding by Clinical Referral Criteria or Predictive Model? . Osteoporos Int 8, 535–539 (1998).
-
Source: https://ilcuk.org.uk/wp-content/uploads/2018/10/OsteoporosisUK.pdf
-
Source: Ji MX, Yu Q. Primary osteoporosis in postmenopausal women. Chronic Dis Transl Med. 2015;1(1):9-13. Published 2015 Mar 21. doi:10.1016/j.cdtm.2015.02.006.
-
Source: https://www.nof.org/preventing-fractures/general-facts/what-women-need-to-know/
-
Source: Stevenson JC. Prevention of osteoporosis: one step forward, two steps back. Menopause International. 2011;17(4):137-141.
Contact My Menopause Centre
- General enquiries: hello@mymenopausecentre.com
- Book appointments online: Log into your account and go to 'My appointments'
- Book appointments by phone: 0333 444 1067
- Website: https://www.mymenopausecentre.com