Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/symptoms/mood-swings/
Menopause and mood swings
Hormone swings, along with the physical and mental symptoms of the menopause can all trigger mood swings. Women still having periods may notice premenstrual syndrome gets worse.
Explore
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An Appointment If you would like to learn more about the impact of your symptom(s) complete our free online menopause questionnaire here.
If you would like to learn more about the impact of your symptom(s) complete our free online menopause questionnaire here.
What are menopause-related mood swings?
Menopausal mood swings can be challenging and upsetting to deal with. Unfortunately, they’re common in the perimenopause and menopause for many of us.
During an episode, you can experience a whole spectrum of emotions, including low mood, anxiety, irritability and anger – and you may find yourself feeling tearful completely out of the blue.
You may feel irrational one minute, then wonder what on earth you were thinking of the next. This can be challenging and upsetting.
 What causes mood swings?
What causes mood swings?
The drop in oestrogen in our bodies is thought to affect how our brain functions through its effect on serotonin and norepinephrine (and likely to be others), substances linked to symptoms of depression.
Oestrogen is linked to serotonin levels (the ‘happy hormone’) in the brain, so that when oestrogen levels drop, so does serotonin[2]. There is evidence that oestrogen is also linked with cortisol levels – the hormone of stress[3] so that when oestrogen levels drop, cortisol levels rise.
Many studies have therefore shown that hormone changes have been linked with changes to mood and anxiety[1].
Lower levels of oestrogen have also been linked to irritability, fatigue, stress, forgetfulness, anxiety, and difficulty concentrating. If this sounds familiar, now you know why.
Some brains are more sensitive to these changing levels of hormones. Decreasing oestrogen levels have been shown to reduce your resilience to, or ability to cope with, stress[4].
Oestrogen isn’t the only hormone involved – testosterone, cortisol and a brain protein called monoamine oxidase A are all also likely to play a role in mood swings.
Sleep – or rather lack of it – can have an impact on your mood. Hot flushes and night sweats commonly affect sleep, so you can see how these things all start to link together. Stress, anxiety and depression can also have an impact, creating a vicious circle. Lack of sleep can make all your other symptoms feel worse.
You may be experiencing stresses at home or work that can affect your mood, at the same time as lower hormone levels which increase your vulnerability and decrease your resilience.
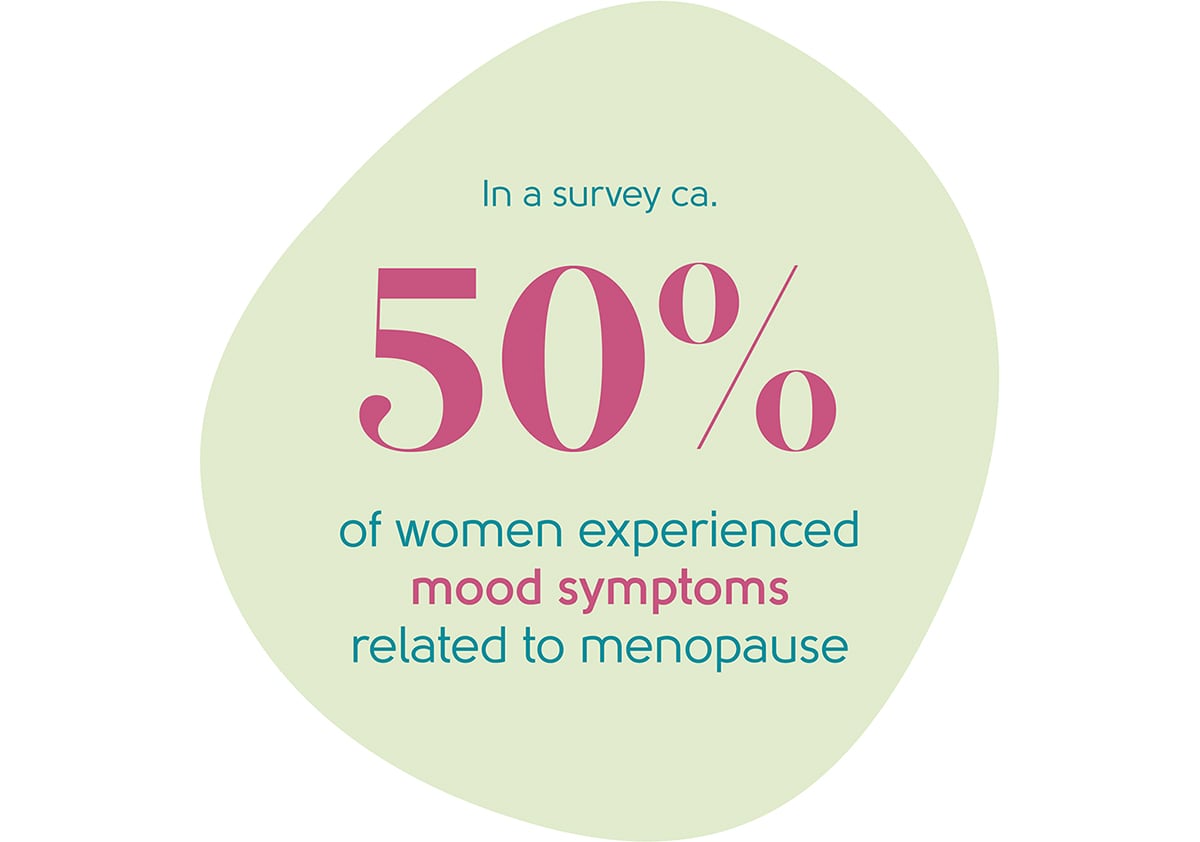
How many women typically experience mood swings?
It is hard to put an exact figure on the number of women experiencing menopause-related shifts in mood. Nevertheless, they are widespread, with a survey by The British Menopause Society showing that over half of the women interviewed experienced symptoms related to mood[5].
Are mood swings linked to any particular stage of the menopause?
Mood swings can be more common in the perimenopause, particularly in the early stages when one of the first signs of your body changing is worsening premenstrual syndrome.
How can mood swings be treated?
Talking to those you live with can really help your mental health. Try explaining that you are experiencing symptoms related to the menopause and that changes in your behaviour are linked to changing hormone levels. Understanding this can help them to be more understanding and tolerant around you.
The best ways to help with mood disorders are similar to those we use to manage depression and anxiety. Recognise your symptoms for what they are – you’re not suffering from a mental illness or losing your old self – you’re simply dealing with hormone swings that affect your brain.
Help for mood swings comes in many forms:
Asking for help
It’s important to talk about how you feel with family and friends, with your doctor, or with a counsellor – someone you trust with a sympathetic ear. Understanding why your mood is low, or why you feel depressed, can go some way to helping find a solution.
If premenstrual syndrome is a particular issue for you, there are other places to look for help and support. The National Association for Premenstrual Syndromes has good information. Other information can be found online through the Royal College of Obstetricians and Gynaecologists.
If you feel suicidal – call your GP practice, the Samaritans 116123, 111 or 999 if you think you are going to harm yourself.
Lifestyle changes
- Cut down on alcohol – alcohol pulls down your mood and affects your sleep. Many women choose alcohol to get them off to sleep, but the quality of sleep can be poor, leaving you feeling tired and irritable the next day.

- Exercise – gentle exercise can work wonders to improve mood, increase your sense of wellbeing, self-worth, body image and feelings of happiness, while reducing stress and anxiety. Our friends at Her Spirit can help you find an activity and provide the support to do it.
- Relaxation – making time to ‘switch off’ is important. Whatever you like to do to relax, build some time into your daily life to do it, and don’t feel guilty about it. Switching off can help to relieve stress and decrease the stress hormones that can affect brain function.
Talking therapies
We sometimes hear women say that they feel guilty or self-indulgent for spending time and money on counselling or coaching. Exploring how you’re feeling (and why) with an objective professional can lift a weight off your shoulders. Any money you spend on this is an investment in yourself, and you’re definitely worth it!
 Cognitive behavioural therapy (CBT) – this can help you sort out how you’re feeling and why, helping you to break the cycle of negativity. Find out more about our CBT partners, Sue Makin, and Claire Lloyd, or our coaching partner, Cognomie.
Cognitive behavioural therapy (CBT) – this can help you sort out how you’re feeling and why, helping you to break the cycle of negativity. Find out more about our CBT partners, Sue Makin, and Claire Lloyd, or our coaching partner, Cognomie.- Counselling – finding a good counsellor can work wonders. It’s a good idea to talk to several before settling on the one for you because finding the right ‘fit’ is essential. BACP is a good place to start, or you could ask your GP for a recommendation.
Hormone Replacement Therapy (HRT)
It’s worth talking to your doctor to find out whether HRT could be suitable for you. If your mood changes are related to the perimenopause or menopause, evidence suggests that HRT may improve mood[6]. It may be worth a try, even for a short time, to see if it helps.
HRT improves the overall quality of life, energy levels and sleep and it does not negatively affect libido or cause sexual dysfunction (which may be affected by antidepressants)[7].
You can find out more about HRT here.
Medication
Antidepressants have a part to play, particularly if you have clinical depression or premenstrual syndrome. They can lift your mood, help you sleep and help with anxiety. Please talk to your doctor about the risks and benefits for you.
If worsening premenstrual syndrome is a particular issue for you, antidepressants can help to lift symptoms, particularly if you have been advised not to or do not want to take hormones. Some antidepressants may also help with treating hot flushes.
What next?
If you’re worried about mood swings in the context of the menopause, see your GP or book an appointment with our menopause clinic.
If you think you may be experiencing symptoms of the menopause transition, you can learn more with our symptom checker or by taking our Menopause Questionnaire.
You can also find more information about the menopause transition at the British Menopause Society and the National Institute for Health and Care Excellence.
Authored by:
Dr Clare Spencer
Registered menopause specialist, GP and co-founder; see Dr Clare in person at The Spire Hospital, Leeds or online
Last updated:
06/11/2023
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentLearn more
Join the pause. community
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Want to be the first to hear our latest news? Join our pause. community today.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Book a consultation
Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowReferences
-
Source: Studd, J, Nappi, RE. Reproductive depression. Gynecol Endocrinol 2012; 28: 42–45; Cohen, LS, Soares, CN, Vitonis, AF, et al. Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry 2006; 63: 385–390.
-
Source: Wharton, W, Gleason, CE, Olson, SR, et al. Neurobiological underpinnings of estrogen-mood relationship. Curr Psychiatry Rev 2012; 8: 247–256.
-
Source: Gordon, JL, Eisenlohr-Moul, TA, Rubinow, DR, et al. Naturally occurring changes in estradiol concentrations in the menopause transition predict morning cortisol and negative mood in perimenopausal depression. Clin Psychol Sci 2016; 4: 919–935.
-
Source: Gordon, JL, Rubinow, DR, Eisenlohr-Moul, TA, et al. Estradiol variability, stressful life events and the emergence of depressive symptomatology during menopause transition. Menopause 2016; 23: 257–266.
-
Source: Currie H, Moger SJ. Menopause – Understanding the impact on women and their partners. Post Reprod Health. 2019 Dec;25(4):183-190.
-
Source: Warren MP. Missed symptoms of menopause. Int J Clin Pract. 2007 Dec;61(12):2041-50. And NICE NG23 2015.
-
Source: Newson, LR. Best practice for HRT: unpicking the evidence. Br J Gen Pract 2016; 66: 597–598.
Contact My Menopause Centre
- General enquiries: hello@mymenopausecentre.com
- Book appointments online: Log into your account and go to 'My appointments'
- Book appointments by phone: 0333 444 1067
- Website: https://www.mymenopausecentre.com


















