Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/blog/hrt-myths-ill-grow-a-beard-and-other-hrt-myths-busted/
‘I’ll grow a beard’ – and other HRT myths busted

To say that Hormone Replacement Therapy (HRT) has had a bad rap over the years is a bit of an understatement. Despite the fact that it has been in use for the treatment of the menopause for over 70 years, there is still confusion and controversy about its risks in particular.
The use of HRT dropped dramatically in the early 2000s when the preliminary findings of the Women’s Health Initiative study were published. The message was put forward loud and clear into the media that HRT caused a number of serious health problems including breast cancer, heart disease and stroke. And so followed years of sensationalist headlines, ‘revelatory’ documentaries, and changes in medical practice.
Fast-forward to today, and a re-working of the data in question – subsequently published – has shown the risks to be smaller, not significant or untrue for most women. Great news – except those myths remain in our national psyche. It’s like anything in life – when a seed of doubt has been planted it’s hard to move on.
So, what IS the truth? Is HRT something we should steer clear of for the sake of our health – or should it be the secret weapon in every menopausal woman’s armoury?
Who better to tell us than our resident HRT expert Dr Clare Spencer. Trust us, what Dr Clare doesn’t know about HRT isn’t worth knowing. Here she reveals all and busts the biggest HRT myths.
Myth #1 ‘HRT causes breast cancer’
Ok, here’s the science bit: as we age, our bodies produce fewer hormones – including oestrogens, progestogens and testosterone, causing everything from hot flushes to low libido. Oestrogen is arguably the most important hormone on this list and HRT aims to replace oestrogen to ease symptoms of the menopause. Some women also need a tiny dose of testosterone to help with their sex drive.
There are two main types of HRT – combined HRT (that’s oestrogen plus a progestogen) and oestrogen-only HRT (normally taken by women who have had a hysterectomy, that is where the womb is removed).
There are also vaginal oestrogens, and these are used to treat vaginal and bladder symptoms such as dryness, soreness, and irritation.
If you take combined HRT, your risk of getting breast cancer is ever so slightly higher but still low. To put that into context, you are more at risk of getting breast cancer in your 50s from lifestyle factors such as being overweight or drinking 2 or more units of alcohol a day (that’s around a double gin or a can of beer) than from taking HRT:
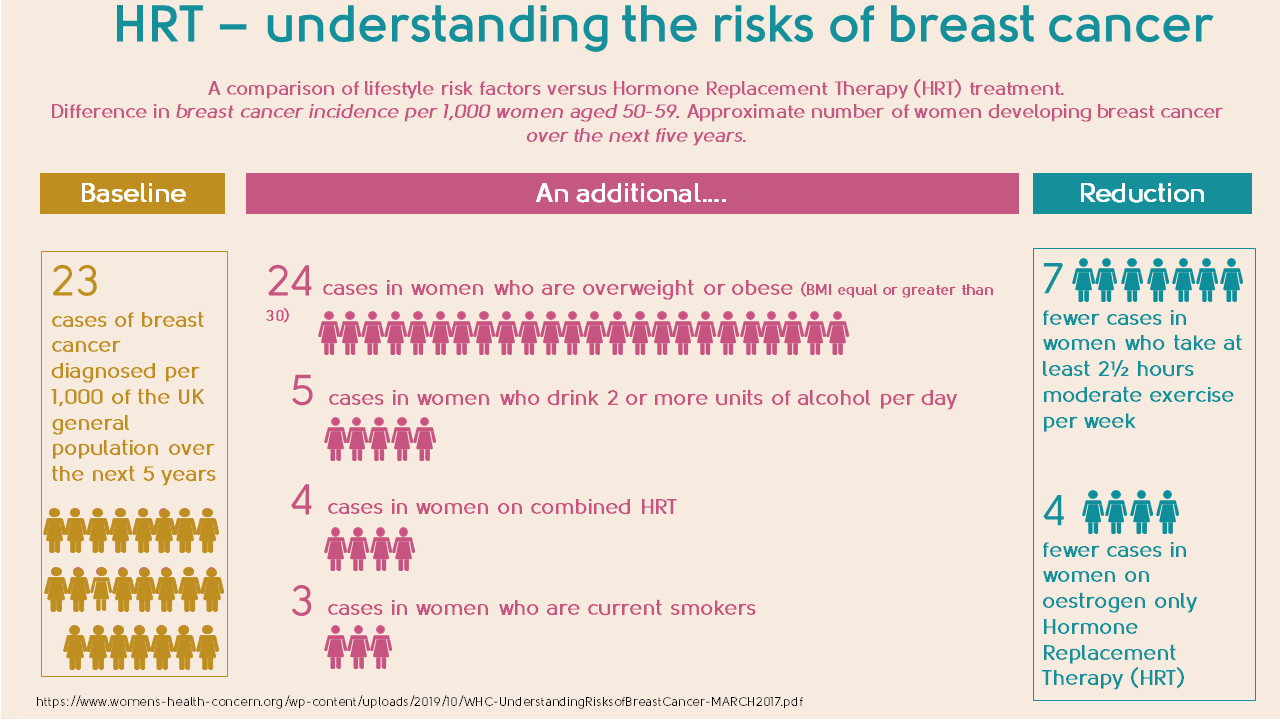
If you are on oestrogen-only HRT (because you have had a hysterectomy), there is little or no increased risk of breast cancer.
You may be wondering why you should take a progestogen then, as your risk of breast cancer is lower if you don’t. Good question. If you haven’t had a hysterectomy and take oestrogen-only HRT this can thicken the lining of your womb, increasing your risk of womb cancer.
You’re prescribed the additional hormone progestogen to protect the lining of the womb and prevent this from happening.
If your HRT is in the form of vaginal oestrogen pessaries, vaginal cream or vaginal gel, you don’t need to take progestogen. It’s a bit confusing, but if you use the oestrogen into the vagina, you only absorb tiny amounts of it, so the risk of cancer doesn’t increase. If you use the oestrogen gel through your skin – like Oestrogel or Sandrena – you absorb more of it and this is when you need to use the progestogen also.
It’s quite a minefield so my advice is always to speak to a menopause expert.
Myth #2 ‘HRT will make me put on weight’
There is no evidence that HRT will make you gain weight. Weight increases with age for many reasons, but there is no evidence that this is linked to HRT. Some women experience fluid retention when they start HRT, but this side effect generally settles with time.
Myth #3 ‘It’s delaying the inevitable’
There is no evidence that HRT presses the pause button on your menopause. Instead, it masks menopausal symptoms while you are taking it. When you decide to stop, you will feel how you were likely to feel at that point in time without having taken HRT.
Myth #4 ‘HRT causes heart disease’
If you start HRT within 10 years of the menopause, or under the age of 60, the risk of heart disease is reduced. HRT tablets (as opposed to patches, gels or spray) slightly increase the risk of stroke. However, it is important to remember that the chance of a healthy woman under 60 having a stroke is very low.
If you’re already at higher risk of cardiovascular disease it may still be possible for you to take HRT but it will depend on your individual circumstances. The best thing is to speak to your doctor or a menopause expert.
Myth #5 ‘My symptoms aren’t ‘bad enough’
Rubbish! You don’t need to wait for severe symptoms to start HRT – it can help even mild symptoms and starting HRT earlier can help prevent heart disease, osteoporosis and fractures. This is particularly if you are under 50.
Myth #6 ‘I suffer from migraines so I can’t have HRT’
While it is true that you may not be able to use combined hormonal contraception if you suffer from migraines, it is likely that you will be able to use HRT. The worry is that migraine sufferers are unfortunately already slightly more at risk of having a stroke and oral HRT increases this risk by a small amount too. Standard doses of oestrogen through the skin – patches, gels or spray – should not increase your risk so, combined with a progestogen, would be a better option.
Myth #7 ‘HRT causes blood clots and strokes’
HRT tablets slightly increase the risk of stroke and blood clots – patches, gels or spray (known as transdermal) don’t. What you need to know though, is that the starting risk is low for fit and healthy women – and so a low risk is increased to a slightly higher low risk. If you prefer to take a tablet, it can still be an option – you just need to understand the benefits and risks and how they apply to you.
The risk of blood clots for anyone are increased with smoking and being obese and increasing age. There are certain medical conditions that also increase risk. If this applies to you, it would be safer to have oestrogen in patches, gels or spray (transdermal). If this applies to you, you may need a discussion with a menopause specialist before starting HRT.
Myth #8 ‘You can only use HRT until you are 60’
For most women, the benefits of HRT outweigh any small risks and they take it happily for many years. Most women do not need to stop taking it because of age alone.
A woman’s chance of developing health conditions such as heart disease, stroke and breast cancer increases with age but this doesn’t mean that HRT has to be stopped when you reach 60. It does mean that the risk of HRT may be decreased by changing from tablet to transdermal form, and the dose of oestrogen may be decreased as most women need less oestrogen to control symptoms.
What’s important is to understand the risks and benefits of HRT and what they mean for you. The benefit and risk balance will vary for every individual woman according to what other risk factors she has. Again my advice is to always speak to your doctor or a menopause expert to help you decide what the best option is for you.
Myth #9 ‘My grandmother has had breast cancer so I can’t have HRT’
Not all family histories of breast cancer are equal. One second degree family member, such as a grandmother, with breast cancer in one breast, diagnosed in old age, is unlikely to affect your risk significantly. Number of relatives affected, age at diagnosis, ancestry and whether one or both breasts were affected are amongst other important factors to take into account also.
If you are unsure about whether your family history of breast cancer affects your risk, speak to your GP – you may need a referral to see a genetics specialist or to a breast cancer family history clinic. It is important that you understand how your family history impacts on your risk.
Even if you are found to have a higher risk of breast cancer, you may be able to take HRT as long as you understand how HRT impacts your risk. You may need to speak to a menopause specialist and gain advice from your breast surgeon to understand this fully.
Myth #10 ‘The higher the dose of HRT, the greater my risk of cancer’
Your doctor will usually start your HRT at a low or standard dose to try and control your symptoms. Some women need to increase the dose to better control their symptoms. As long as you stay within standard doses, there is no evidence that your risk of breast cancer increases with the change of dose. And there is no evidence that the risk of breast cancer depends on whether you take HRT as tablet, patch or gel form.
Myth #11 ‘You can only take HRT for 5 years’
You can take HRT for as long as you would like, as long as you understand the benefits and risks and how they apply to you. A good menopause expert should explain your treatment clearly to you so you feel empowered to make the right choices.
Myth #12 ‘I can only start HRT once my periods have stopped for a year’
Some women experience menopausal symptoms such as anxiety, hot flushes and mood swings before their periods have stopped. If this is you, you can absolutely start HRT. You would need to have sequential HRT, which gives a regular withdrawal bleed – read more about HRT. If you don’t want to continue having regular bleeds, you could consider having a Mirena™ intrauterine system (coil) fitted – this will provide you with the progestogen part of your HRT and you can take the oestrogen separately.
Myth #13 ‘I’m in my 40s so I must be too young to take HRT’
Most women begin the perimenopause, and start menopause symptoms, in their mid-to-late 40s, but can it be earlier: 1% of women under the age of 40 go through the menopause and 5% by the time they are 45. So you can never be ‘too young’ – it all depends on what’s going on in your body.
If you are going through a premature or early menopause, a discussion about HRT is important. Not only does it ease symptoms, but it will also help prevent osteoporosis, heart disease and the decline of brain function. Taking HRT under the age of 50 is unlikely to significantly increase your risk of breast cancer – for most the benefits far outweigh any small risks.
Myth #14 ‘I hate taking tablets so HRT isn’t for me’
HRT comes in patches, gels, sprays and also the Mirena™ coil – if you don’t want to take a tablet you don’t have to.
Myth #15 ‘I can’t use vaginal oestrogen creams or pessaries to help with vaginal dryness or bladder symptoms if I am taking HRT’
You can! Around a quarter of women using HRT also need vaginal oestrogen to help with vaginal dryness, irritation and painful sex and bladder symptoms of the menopause also. There is no known additional risk from adding in a vaginal oestrogen as the absorption into your body is tiny.
Myth #16 ‘Taking testosterone will give me facial hair’
Most women are surprised to hear that testosterone, as well as oestrogen, naturally occurs in our bodies and around half of our testosterone is made by our ovaries.
This male hormone contributes to sex drive, arousal and orgasm. It’s also important for muscle and bone strength, mood and how our brain functions as well as maintaining health of the tissues of the vulva, vagina and bladder. The levels of testosterone decline slowly and gradually during our adult life.
While oestrogen-containing HRT helps many, adding in testosterone can be the missing piece of the jigsaw for others. You only need to take a tiny amount – not enough to cause male changes, such as significant facial hair growth that many worry about.
Myth #17 ‘The hormones I buy privately are better than conventional prescriptions’
Many women think that they can only get bioidentical hormones by seeing a doctor privately and this is definitely a myth. There are two types of bioidentical HRT. There is conventional, prescribed bioidentical HRT that is available through the NHS or private clinics (like ours.) Then there are compounded bioidentical hormones that rely on blood tests and are not regulated in the same way that a conventional prescription is. There is no evidence that these compounded forms of HRT are any more effective or as safe as hormones that are conventionally prescribed.
Myth #18 I can’t get pregnant if I am taking HRT
You absolutely can! HRT is not birth control unless you use the Mirena™ intrauterine system (coil) as part of your HRT. You can take contraception alongside HRT though, and all women can stop contraception when they reach 55.
If you’re interested in learning more about HRT, we’ve lots of more information here.
Authored by:
Dr Clare Spencer
Registered menopause specialist, GP and co-founder; see Dr Clare in person at The Spire Hospital, Leeds or online
Last updated:
20/12/2022
Join the pause. community
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Want to be the first to hear our latest news? Join our pause. community today.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Book a consultation
Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowContact My Menopause Centre
- General enquiries: hello@mymenopausecentre.com
- Book appointments online: Log into your account and go to 'My appointments'
- Book appointments by phone: 0333 444 1067
- Website: https://www.mymenopausecentre.com



















We’d love to hear from you
Please ensure you’re logged in to leave a comment. Not got an account – registration is quick and easy! All comments are moderated prior to being posted on the website and are subject to our Acceptable Use Policy.
Comments