Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/symptoms/period-changes/
Menopause and period changes
Periods can become irregular – heavier, lighter, more or less frequent – in the perimenopause and in the menopause they stop completely.
Explore
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentIf you would like to learn more about the impact of your symptom(s) complete our free online menopause questionnaire here.
What are menopause-related period changes?
One of the most noticeable symptoms of the perimenopause and menopause is that your normal bleeding pattern can change. Most of us are used to having monthly bleeds, although some women have more irregular periods.
As you start your menopause transition, you may start to experience any of the following changes:
- You might begin to miss periods
- They may become lighter
- They might become heavier or longer – leaving you feeling drained and tired
- They may even become more frequent
- You might pass clots or experience flooding, where the period comes out with a gush
- For some women, they can just stop out of the blue.

It’s worth remembering that many women take hormones for contraception that can also change their periods. For example, many women don’t bleed, or experience changes to their pattern of bleeding, with the Mirena™ coil, progesterone-only pill, implant or contraceptive injection. The combined oral contraceptive pill can keep your menstrual periods regular even through the perimenopause.
So if you’re taking hormones, you can’t rely on changing bleeding patterns to work out whether or not you’re in the perimenopause or if you’ve been through the menopause.
What causes period changes?
Having a regular monthly bleed relies on several hormones (chemical messengers) working together.
Your brain and ovaries communicate to keep your hormones in a monthly cycle. Hormones from the ovary (oestrogen and progesterone) cause changes to the lining of the womb (called the endometrium), so that every month it thickens (just in case it needs to look after a pregnancy). Then, if you’re not pregnant, it sheds – this is the bleeding you see with a period.
In the perimenopause, your hormones can become out of sync and communication between your brain and ovaries breaks down. That regular thickening and shedding of your womb lining doesn’t happen.
Bleeding can become erratic, or you may not get any at all. In the menopause, when oestrogen levels are low, the lining of the womb stops thickening and bleeding stops.
There are other reasons for abnormal bleeding, such as fibroids, polyps in the lining of the womb (endometrial polyps), and – more rarely – precancerous and cancerous changes. Bleeding can also come from the cervix – that’s why it’s essential to keep up to date with your cervical smears – as well as from the vagina and vulva.
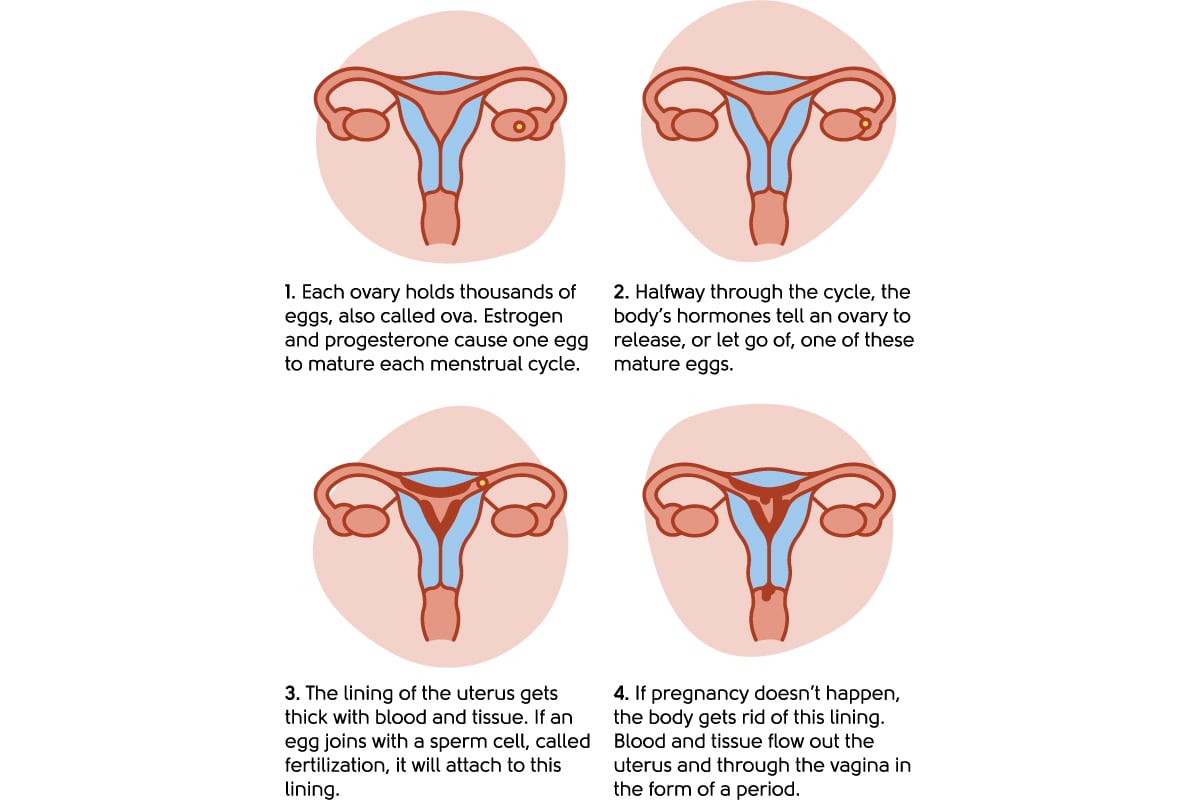
Illustration to show the menstrual cycle
Postmenopausal bleeding
Some women experience vaginal bleeding after menopause – that is bleeding after your periods have stopped for more than 12 months. This is called postmenopausal bleeding. Bleeding after the menopause always needs to be checked by a doctor, even if it has only happened once and even if it’s spotting or looks brown or pink.
The cause of postmenopausal bleeding is usually not serious, but it can be a sign of cancer. This type of cancer is easily treated if found early.
The most common cause of postmenopausal bleeding is that the tissues of the vulva, vagina, cervix or womb lining have become thin and delicate, making them more prone to bleeding. There are other causes too, such as polyps on the cervix or womb lining. These are small growths that are usually not cancerous.
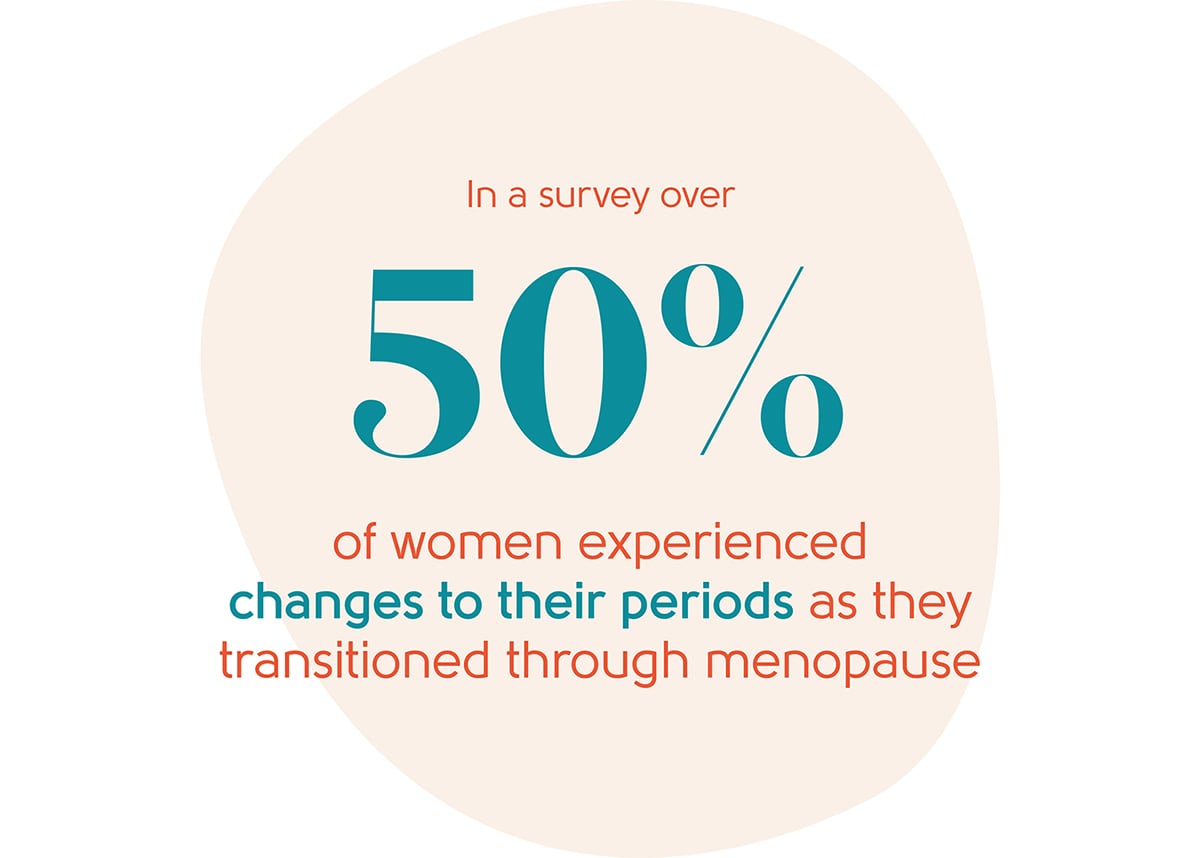
How many women typically experience period changes?
In a survey by the British Menopause Society, over 50% of the women interviewed reported changes to their periods [1].
Are period changes linked to any particular stage of the menopause?
 Period changes related to the menopause start in the perimenopause. The perimenopause typically starts up to eight to ten years before the menopause (though it can be shorter) and usually in your mid-to-late 40s (but for some it can be earlier or later).
Period changes related to the menopause start in the perimenopause. The perimenopause typically starts up to eight to ten years before the menopause (though it can be shorter) and usually in your mid-to-late 40s (but for some it can be earlier or later).
Many women will be taking hormones to help regulate their periods, either as contraceptives or to treat heavy periods or endometriosis. So if you’re taking hormones, you can’t rely on changing bleeding patterns to work out whether or not you’re in the perimenopause or if you’ve been through the menopause.
Ultimately, all women who are having periods will go through the menopause, where their periods will stop. The average age for the menopause in the UK is 51, and by the age of 55, most women will have naturally stopped having periods.
How can period changes be treated?
You should see a doctor if:
- You have bleeding that has become heavier
- Your periods are lasting longer
- You are bleeding in between periods
- You have vaginal bleeding after sex during the menopause
- If you haven’t had a bleed for a year or more and then start bleeding again
You may also need a full blood count and a check of your iron levels.
Irregular and heavy bleeding can go on for years in the perimenopause. You may want to consider treatment to stop or lighten your periods. There are hormonal and non-hormonal options to help with this:
Non-hormonal options
- Tranexamic acid – This is a tablet that you take just while you’re bleeding. It can be effective in ‘turning down the tap’ and making periods lighter.
- Mefenamic acid – This is a tablet similar to ibuprofen and aspirin that can also be effective in making bleeding lighter and it’s good for period pain. You take this just before and during bleeding.
Both of these options can be prescribed by GPs, or in our menopause clinic.
Hormonal options
- The progesterone-only pill – An option that’s helpful for some women who have heavy periods, although some have more frequent bleeding. It’s easy to start and stop as it’s just a tablet. It’s also a contraceptive but is not licensed for use as part of HRT.
- The combined pill – This can still be an option for some women if you’re under the age of 50.
- Sequential HRT – This type of HRT can be helpful in regulating bleeding. It causes a monthly bleed by overriding your hormones. You can find more information about HRT here.
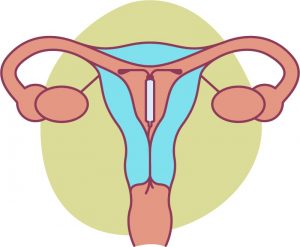 The Mirena™ coil – This can be very effective and is a small, T-shaped plastic device that’s fed through the cervix to sit inside the cavity of the womb. It releases a tiny amount of hormone called levonorgestrel (a progestogen) that keeps the lining of your womb thin. After a year with one of these coils, most women have only occasional periods or no periods. A Mirena™ lasts for five years and has other effects too – it’s a contraceptive and can be used as part of Hormone Replacement Therapy (HRT). See our information sheet to read more about Mirena™ coils. It can be a great option for many women.
The Mirena™ coil – This can be very effective and is a small, T-shaped plastic device that’s fed through the cervix to sit inside the cavity of the womb. It releases a tiny amount of hormone called levonorgestrel (a progestogen) that keeps the lining of your womb thin. After a year with one of these coils, most women have only occasional periods or no periods. A Mirena™ lasts for five years and has other effects too – it’s a contraceptive and can be used as part of Hormone Replacement Therapy (HRT). See our information sheet to read more about Mirena™ coils. It can be a great option for many women.
You can find out more about contraception here.
Other options and procedures
If you are referred to a gynaecologist, they may talk to you about endometrial ablation (lining of the womb ablation). This is a surgical treatment to treat heavy periods (menorrhagia). During the procedure, most of your womb lining (endometrium) will be destroyed or removed. This may stop your periods completely or they may become lighter. Having a hysterectomy for bleeding issues alone is an absolute last resort.
Finally, if your bleeding has suddenly stopped, don’t forget to do a pregnancy test if you’re sexually active and there is the possibility of pregnancy.
What next?
If you’re concerned about period changes, see your GP, gynaecologist, or book an appointment with our menopause clinic. As we are an online clinic, we can’t fit Mirena™ coils. Many GPs and nurses fit Mirena™ and you can usually get this done at your GP practice or a local sexual health clinic.
If you think you may be experiencing symptoms of the menopause transition, you can learn more with our symptom checker or by taking our Menopause Questionnaire.
You can also find more information about the menopause transition at the British Menopause Society and the National Institute for Health and Care Excellence.
Authored by:
Dr Clare Spencer
Registered menopause specialist, GP and co-founder; see Dr Clare in person at The Spire Hospital, Leeds or online
Last updated:
07/04/2021
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentLearn more
Join the pause. community
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Want to be the first to hear our latest news? Join our pause. community today.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Book a consultation
Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowReferences
-
Source: Currie H, Moger SJ. Menopause – Understanding the impact on women and their partners. Post Reprod Health. 2019 Dec;25(4):183-190.
Contact My Menopause Centre
- General enquiries: hello@mymenopausecentre.com
- Book appointments online: Log into your account and go to 'My appointments'
- Book appointments by phone: 0333 444 1067
- Website: https://www.mymenopausecentre.com