Downloaded from www.mymenopausecentre.com
Direct URL: https://www.mymenopausecentre.com/gp-resources/the-key-things-you-need-to-know-about-progestogens-and-progesterone/
The key things you need to know about progestogens and progesterone
In this article our co-founder, registered menopause specialist and GP, Dr Clare Spencer, explains what progesterone is, why - for most women - it’s important as part of your HRT regime, and the alternatives if you find it difficult to take or you cannot find UtrogestanTM because of any supply shortages.
Explore
- What does progesterone do?
- Why is a progestogen needed in HRT?
- Are blood tests helpful to check progesterone levels?
- Side effects of progestogens
- Progestogens and breast cancer risk
- Commonly used progestogens in HRT
- What are your options if you cannot get your usual prescription of oral UtrogestanTM capsules?
- What can you do if you have progesterone and progestogen sensitivity?
- Share
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentOestrogen is commonly talked about as being the most important sex hormone for women, but the ovaries make another hormone – progesterone – and many women need this to form part of their hormone replacement therapy (HRT) also.
Before we look at what progesterone does, it’s helpful to understand the different terminology used, which can be confusing:
- Progesterone is the name of the hormone made by cells in the ovaries. Utrogestan oral capsules contain the ‘body identical’ progesterone.
- Progestogens (or sometimes the term progestins is used) are versions of progesterone. They are synthetic hormone drugs that mimic the body’s own progesterone. Many types of HRT (and the combined oral contraceptive pill) contain a synthetic progestogen (for example norethisterone, dydrogesterone, medroxyprogesterone acetate or levonorgestrel in the Mirena or Levosert coils). They all do a similar job, but the side effects can vary.
Through this article, we will refer to progestogens to include synthetic and body-identical hormones.
What does progesterone do?
During reproductive life, from puberty to the menopause transition, the most important activity of progesterone is to prepare the womb lining for pregnancy during the second half of the menstrual cycle (called the luteal phase).
If there is a pregnancy – if the egg released is fertilised by a sperm – the progesterone is important for maintaining that pregnancy. Amongst other actions, it allows the womb lining to ‘mature’ so it is ready to allow the fertilised egg to implant and develop.
Look at the diagram below to see how the progesterone levels (shown in green) change during the monthly cycle – if a pregnancy does not happen, the progesterone level drops and the womb lining is shed.
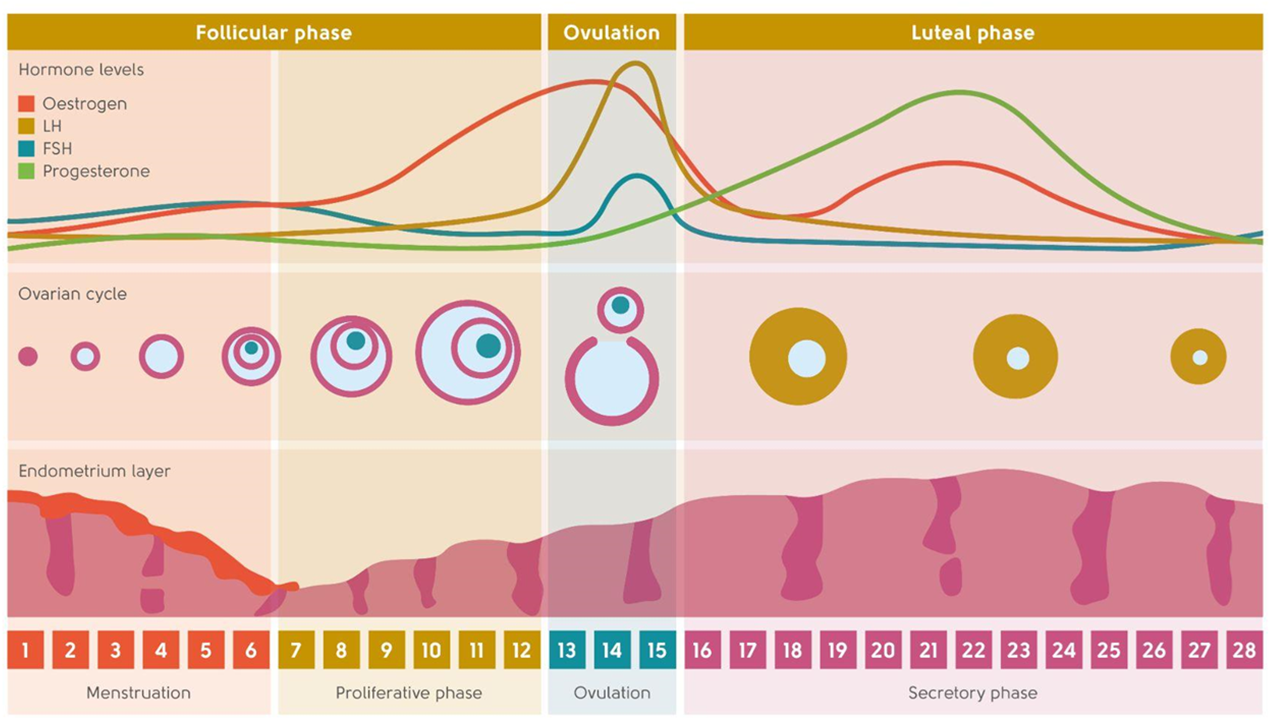
In addition, progestogens can have an impact on mood and behaviour and they also have a role to play in maintaining bone density– helping to keep the bones strong and less likely to fracture as a result.
Why is a progestogen needed in HRT?
Oestrogen is needed to manage most menopause symptoms. If you still have a womb (you have not had a hysterectomy) and take oestrogen by itself, this can thicken the lining of your womb, increasing your risk of womb cancer. The progestogen hormone is there to protect the lining of the womb, keeping it stable and preventing it from over thickening. If you had a subtotal hysterectomy or if you had a hysterectomy for endometriosis, you may also need a progestogen alongside oestrogen. This will be discussed with you.
It is so important, therefore, to speak to a doctor or other healthcare professional if you are not tolerating the progestogen in your HRT or if you cannot get access to your usual prescription due to shortages through your pharmacy.
You can read more about how progestogens fit into HRT here.
Are blood tests helpful to check progesterone levels?
Blood tests for progesterone do not have a role in menopause management. We use set doses of progestogen and progesterone that have been shown to keep the womb lining thin.
A blood test won’t help predict side effects and won’t tell us if your side effects are progestogen related.
The only use of blood tests for progesterone is to check to see if you have ovulated – that is to find out if you have released an egg during the menstrual cycle that can then become fertilised by sperm. This blood test should be timed to be taken 7 days before your period.
Side effects of progestogens
How do progestogens effect mood?
For some women, progestogens and progesterone can significantly impact mood. For example, the rise in progesterone and, for some, the drop before a period, can be the cause of premenstrual syndrome (PMS)-like symptoms.
Some women experience symptoms when they take progestogens in HRT and contraception pills with varying degrees of severity – some feel irritable and low, while others can feel very depressed.
We don’t know exactly why some women are more sensitive to progestogens than others.
It’s likely that the impact on mood occurs as progestogens can have an effect on the chemicals in our brain that are responsible for controlling levels of mood and anxiety, for example serotonin and GABA (gamma aminobutyric acid – thought to play a role in controlling anxiety, stress and fear).
Mood related side effects include tension and irritability, fatigue, feelings of aggression or anger, mood swings, anxiety and loss of confidence.
When you give a progestogen in HRT, some women feel great. The micronized progesterone in oral UtrogestanTM capsules can help get you into a deeper state of sleep and can take the edge off anxiety.
However, other women may have side effects such as a lower mood or irritability. Side effects can improve over time. Some tolerate one type of progestogen and not others. A small percentage of women do not tolerate the progestogen or their own progesterone at all. They feel very low, as if a dark cloud is hanging over them, and feel depressed. Some even feel suicidal (and see below for a link to support if this is happening to you). These symptoms usually lift when the progestogen is stopped – and this is how you can tell the difference between progestogen sensitivity and clinical depression. Unfortunately, we don’t yet have a test to find out who will be sensitive to progestogens and who won’t. It is so important that you talk to your doctor if you are experiencing these symptoms so you can discuss alternatives, to find a progestogen that does suit you, or a way of taking it that can be tolerated. A menopause specialist is the ideal person to talk to about this (if you would like to book an appointment with one of the menopause specialists in our clinic, head here).
It is important to understand that the fewer than recommended number of days that a progestogen is taken each month, the greater the risk of womb lining thickening, and a way of monitoring this may need to be discussed if you are not able to tolerate taking the progestogen as recommended.
What are the physical side effects of progestogens?
Physical side effects include breast tenderness, bloating, headaches/migraine, acne/greasy skin, constipation, nausea and fluid retention – all very similar to premenstrual symptoms for some women.
Progestogens and breast cancer risk
The risk of breast cancer as a result of taking HRT has been shown to vary with the type of progestogen used, though the differences are very small, and the absolute level of risk is very small. [1] [2] [3]
In general, the risk of breast cancer with body-identical progesterone or dydrogesterone (biochemical very similar to body-identical progesterone) seems to be lower than with synthetic alternatives such as medroxyprogesterone acetate and norethisterone. However, the risk is still very low with the synthetic alternatives.
If you’ve looked at the National Institute of Clinical Excellence guidelines on menopause (here), you will see that oestrogen-only HRT has little or no change in the risk of breast cancer and HRT with oestrogen and progestogen can be associated with an increase in the risk of breast cancer. The risk is small and is balanced against the greater increase in the risk of cancer of the womb if the progestogen is not taken.
The National Institute of Clinical Excellence (NICE) state in their guidance on the menopause that:
- the baseline risk of breast cancer for women around menopausal age varies from one woman to another according to the presence of underlying risk factors
- HRT with oestrogen alone is associated with little or no change in the risk of breast cancer
- HRT with oestrogen and progestogen can be associated with an increase in the risk of breast cancer
- any increase in the risk of breast cancer is related to treatment duration and reduces after stopping HRT
However, the risk of cancer of the womb lining is greater if the progestogen is not taken.
Commonly used progestogens in HRT
The progestogens discussed below are available to take alongside your oestrogen. Some women will tolerate one but not the other, other are better for controlling bleeding than others – there is variability in both tolerance and effect.
Micronised progesterone
Micronised progesterone is biochemically matched to your own progesterone – so it’s bioidentical – and is available on prescription as a small capsule that is usually swallowed, called UtrogestanTM, in addition to oestrogen.
Compared to synthetic progestogens (which are versions of the same hormone), micronised progesterone has several advantages:
- it is often better tolerated
- it can help with sleep
- there is evidence that the risk of breast cancer is lower when compared with synthetic alternatives
Unlike synthetic progestogens, micronised progesterone should not affect your risk of heart disease or blood clotting.
The case of the capsule contains soy and gelatin. If you have a severe nut allergy, some women are allergic to soy may not be suitable for you. The gelatin is usually of bovine origin and therefore not suitable for vegans/vegetarians or some religious groups.
You can read more about UtrogestanTM here.
Using micronised progesterone vaginally
Micronised progesterone can be used vaginally, off license. A pessary (or the oral capsule as a last resort) of progesterone is inserted into the vagina where it is absorbed by the blood vessels that surround the vagina. There is evidence, albeit limited, that it is effective in keeping the womb lining thin and stable when taken this way. Some women tolerate progesterone better when it is absorbed vaginally. This is because the breakdown products of progesterone are the ones usually impacting on mood, and there are more of the breakdown products when progesterone is swallowed compared with when it is used vaginally.
BijuveTM
BijuveTM is a combined oral capsule containing 1mg oestradiol and 100mg micronized progesterone and is an option for women who want to take body-identical progesterone plus oestrogen in 1 oral capsule. The shell contains gelatine.
Medroxyprogesterone acetate
Medroxyprogesterone acetate (MPA) is the progestogen found in ProveraTM. This is a synthetic progestogen and comes in the form of a small tablet that can be swallowed separately from the oestrogen which would then be taken as gel, patch spray or tablet. There is one combined oral HRT called IndivinaTM which contains both oestrogen and MPA, though at the time of writing, there are stock issues with this.
While ProveraTM is not licensed to take separately as part of HRT, it is used frequently for this purpose. It is licensed to use as a treatment for endometriosis and abnormal bleeding.
Levonorgestrel
Levonorgestrel is the synthetic progestogen found in the Mirena™ intrauterine system or ‘coil’, the Levosert™ coil and Femseven™ patches – Femseven Conti and Femseven Sequi.
The Mirena is a small T-shaped device that sits in the cavity of the womb and releases a tiny amount of levonorgestrel into the womb lining and blood stream.
Once a Mirena™ has been fitted, it lasts for 5 years (this use is outside its product license – but is used in line with guidance from the Faculty of Sexual and Reproductive Healthcare). The advantage of having a Mirena fit is that it provides contraception for those who need it, for most women it will stop bleeding if you are still having periods when it is fit, and it is a good way of managing the unpredictable, heavy bleeding than some women suffer in the perimenopause.
A Mirena does not suit everyone, but if it does suit you, it is a very convenient way of delivering the progestogen and, for HRT, all you need is to use the oestrogen alongside in patch, gel, spray or tablet. The other advantage of the Mirena is that the amount of progestogen absorbed is tiny, so it may be better tolerated than progestogens that are swallowed or absorbed through the skin.
The Levosert™ coil contains the same amount of levonorgestrel as the Mirena™. It has a license for contraception and treatment of heavy menstrual bleeding but does not have a license for use in HRT. Although Mirena™ is currently the only LNG-IUD that is licensed for this indication, the FSRH supports the use of any 52 mg Intrauterine contraception for endometrial protection as part of HRT for up to 5 years. This recommendation is supported by the Royal College of Obstetricians and Gynaecologists and the British Menopause Society[2].
Femseven patches are patches that you change weekly rather than twice weekly. The levonorgestrel is absorbed through the skin in the combined patches. At the time of writing, there are supply issues with Femseven Sequi patches but Fenseven Conti should be available.
The risk of breast cancer as a result of taking levonorgestrel in the Mirena is not zero, but it is low [3].
Dydrogesterone
Dydrogesterone is very similar in biochemical structure to micronized progesterone. In the UK it is only possible to take it mixed with oestradiol in the Femoston™ products – it is not available separately.
Dydrogesterone may be better tolerated than other synthetic alternatives as it is so close to progesterone. Like micronized progesterone, there is evidence from observation studies that the risk of breast cancer is lower than more synthetic alternatives (such as MPA and norethisterone.)
There is lactose in the combined HRT Femoston tablets.
Norethisterone
Norethisterone is a synthetic progestogen that is biochemically similar to testosterone – more so than other progestogens. It is found in Evorel Conti and Evorel Sequi twice-weekly patches plus some brands of combined oral HRT which it is taken with oestradiol – e.g. Elleste Duet and Ellest Duet Conti, Kliofem and Kliovance. In addition, it can be taken separately to protect the womb lining. It is also found in some progesterone-only contraceptive pills – e.g. Noriday.
Some women do not tolerate norethisterone so well, experiencing irritability headaches and fluid retention.
Norethisterone taken orally may increase the risk of blood clots by a small amount. It is an effective way of managing heavy or unscheduled bleeding. On its own (i.e., not in a combined tablet) it is not licensed for use as part of HRT, but it can be, and is, used in this way. It is not recommended to take it as part of HRT if your body mass index is 30 or above because of the risk of blood clots.
Like other tablets, lactose is found in norethisterone tablets. There is a marginally higher risk of breast cancer compared with micronised progesterone and dydrogesterone, but it is effective in managing troublesome bleeding and it is convenient to use the combined pills.
Desogestrel
Desogestrel is a synthetic progestogen found in Cerazette™ and Cerelle™ progesterone-only pills (POP). It is not licensed to use as part of HRT. There are studies to show that desogestrel 150 micrograms may be effective as the progestogen component of HRT for some women (i.e., 2 x Cerazette/Cerelle 75mcg POP). There is a lack of evidence to show that desogestrel 75 micrograms on its own is adequate and if you are using this for contraception, an additional progestogen would need to be added[4].
Desogestrel is well tolerated by some women and not by others. There is lactose in the tablet ingredients. Off license, therefore, and accepting the lack of large studies, a double dose of desogestrel – 15mcg – can be used for continuous combined HRT and contraception.
Livial™
Livial™ is tibolone – a synthetic form of HRT that mimics the activity of oestrogen and progestogens – and may also have some androgen (male hormone) activity. It can be an option if you do not tolerate progesterone or other progestogens and is usually taken as a form of HRT when your periods have stopped. For more info, head here.
What are your options if you cannot get your usual prescription of oral UtrogestanTM capsules?
You should discuss the following options with your doctor:
- Have a Mirena or Levosert coil fit. Although having a coil fit may not be the most pleasant of experiences once it is in, it can stay in for 5 years and they are usually much easier to remove if you really do not tolerate it.
- Switch to a combined patch – Evorel Conti or Evorel Sequi, or Femseven Conti or Femseven Sequi (if available).
- Use Provera (medroxyprogesterone acetate) tablets or norethisterone tablets separately to the oestrogen.
- Speak to your doctor or other healthcare professional about whether using a micronized progesterone pessary would be a suitable method for you.
- Again, speak to your doctor or other healthcare professional about whether a double dose of desogestrel containing POP would be suitable for you.
- If you are perimenopausal and under the age of 50, the combined oral contraceptive pill could be an alternative. Not everyone can take this – for example, if you smoke the risks would be deemed to be high in relation to the benefits. It may be an option for some, however, and be useful if you need contraception also (you can read more here).
What can you do if you have progesterone and progestogen sensitivity?
If you are sensitive to taking progesterone/progestogen, please don’t despair. It’s really important that you speak to a healthcare professional or one of the menopause specialists in our clinic to discuss your options.
You are not alone
Remember, if you are having dark thoughts or feel suicidal please call your GP practice, the Samaritans, 111 or 999 straight away.
Further reading
Hormone Replacement Therapy explained
Authored by:
Dr Clare Spencer
Registered menopause specialist, GP and co-founder; see Dr Clare in person at The Spire Hospital, Leeds or online
Book an appointment
The highly experienced doctors and nurses in our menopause clinic are here to help you. Appointments from £190.
Book An AppointmentJoin the pause. community
We’ve created pause. as a space for women to come together and share stories about their menopause experience, ask questions, and to find support and inspiration. We'll also share the latest news and updates on the menopause from our experts.
Want to be the first to hear our latest news? Join our pause. community today.
Share your email to receive the latest news, updates and information on new products and treatments from My Menopause Centre and our pause. community. You can unsubscribe at any time.
We're committed to protecting and respecting your privacy - see our Privacy Policy and Terms and Conditions

Book a consultation
Whether you want to discuss your symptoms, create a treatment plan that's right for you, understand some test results or have a check-up, the highly experienced doctors and nurses in our menopause clinic are here to help you.
Book nowReferences
-
See Fournier A, Berrino F, Clavel-Chapelon F. Unequal risks for breast cancer associated with different hormone replacement therapies: results from the E3N cohort study. Breast Cancer Res Treat. 2008 Jan;107(1):103-11. doi: 10.1007/s10549-007-9523-x. Epub 2007 Feb 27. Erratum in: Breast Cancer Res Treat. 2008 Jan;107(2):307-8. PMID: 17333341; PMCID: PMC2211383.
-
FSRH Guideline (March 2023) Intrauterine contraception | BMJ Sexual & Reproductive Health
-
Fitzpatrick D, Pirie K, Reeves G, Green J, Beral V (2023) Combined and progestagen-only hormonal contraceptives and breast cancer risk: A UK nested case–control study and meta-analysis. PLoS Med 20(3): e1004188. https://doi.org/ 10.1371/journal.pmed.1004188.
-
Langer RD, Hobis HN, Lobo RA et al. Hormone replacement therapy- where are we now? Climacteric. 24:1 3-10
-
The British Menopause Society and Womens Health Concern 2020 recommendations on hormone replacement therapy in menopausal women. Post Reproductive Health 2020 26(4) 181-208
Contact My Menopause Centre
- General enquiries: hello@mymenopausecentre.com
- Book appointments online: Log into your account and go to 'My appointments'
- Book appointments by phone: 0333 444 1067
- Website: https://www.mymenopausecentre.com


















